Anticholinergic Risk Calculator
What is the Anticholinergic Cognitive Burden (ACB) Score?
The ACB scale measures the anticholinergic burden from your medications. A score of 1 indicates a drug with minimal risk, while scores of 2 or 3 indicate higher risk. The higher your total score, the greater your risk of urinary retention and cognitive side effects.
Select medications you're currently taking to calculate your total anticholinergic burden score:
Imagine taking a pill to help with frequent bathroom trips, only to find yourself completely unable to urinate. No warning. No gradual warning. Just sudden, painful blockage-and a catheter needed to save you. This isn’t rare. It happens more often than most doctors admit, especially in men over 65. And the culprit? Common medications prescribed for overactive bladder, allergies, depression, and even sleep problems: anticholinergics.
How Anticholinergics Break Your Bladder
Your bladder doesn’t work like a toilet you flush. It’s controlled by nerves and muscles that rely on a chemical called acetylcholine. When it’s time to pee, acetylcholine tells the bladder muscle (detrusor) to squeeze and push urine out. Anticholinergic drugs block this signal. They’re designed to calm an overactive bladder by reducing unwanted contractions. But they don’t know the difference between a spastic bladder and a normal one that just needs to empty. The problem? These drugs hit the M3 receptors in your bladder-the ones that actually make the muscle contract. Even if you have a perfectly healthy bladder, blocking M3 receptors can leave you with urine stuck inside. That’s urinary retention. And once it starts, it doesn’t always go away on its own.Who’s at Risk? The Hidden Vulnerable Groups
Not everyone gets urinary retention from these meds. But some people are sitting ducks. Men over 65 with even mild prostate enlargement are at the highest risk. A 2019 study from the University of Calgary found that in this group, the chance of drug-induced retention jumps from 0.5% in the general population to 4.3%. That’s more than 1 in 25 men. Why? Because their prostate is already squeezing the urethra. Add an anticholinergic on top, and the bladder can’t push through. It’s like trying to squeeze toothpaste out of a tube that’s half-pinched shut. Women aren’t immune. But men are far more likely to need emergency catheterization. A 2022 survey of 1,234 anticholinergic users found 12.3% of men experienced retention severe enough to require a catheter-versus just 5.1% of women. Older adults with dementia or cognitive decline are another high-risk group. The Beers Criteria, used by doctors across the U.S. and Europe, lists anticholinergics as “potentially inappropriate” for seniors because they increase the risk of urinary retention, confusion, falls, and even death. One 2016 JAMA study showed anticholinergic use raised retention risk by 49% in elderly patients with dementia.Not All Anticholinergics Are Created Equal
You might think all drugs in this class are the same. They’re not. The risk varies wildly depending on the specific drug. - Oxybutynin (Ditropan, Oxytrol): High risk. It blocks M1, M2, and M3 receptors equally. In men with BPH, it carries a 3.2 times higher risk of retention than placebo. Its oral form is especially dangerous. The patch reduces risk by 42%, but it’s still not safe for high-risk patients. - Tolterodine (Detrol): Lower risk than oxybutynin. A 2001 study of over 3,000 men found oxybutynin caused 2.1 times more retention than tolterodine. - Solifenacin (Vesicare): More selective for M3 receptors. Still carries a 1.2-1.8% risk of retention, but better than oxybutynin. - Trospium chloride (Sanctura): Doesn’t cross the blood-brain barrier easily. Lower risk of brain fog, but still carries a 1.5-2.2% retention risk. - Darifenacin (Enablex): Very selective for M3. Slightly safer, but still not risk-free. The Anticholinergic Cognitive Burden (ACB) scale helps doctors measure total risk. If you’re taking multiple drugs with ACB scores of 2 or 3-like an antihistamine, a sleep aid, and an OAB pill-your total burden can push you into the danger zone. A 2017 study found patients with a total ACB score of 3 or higher had a 68% higher risk of urinary retention.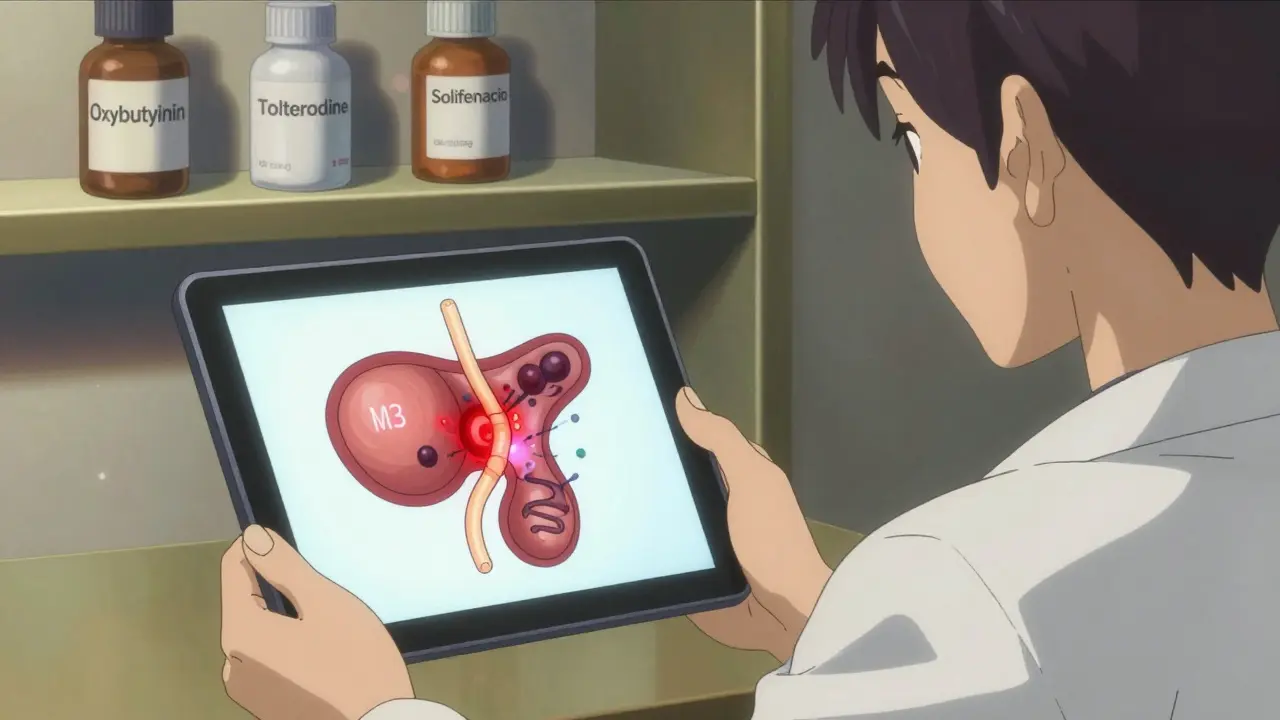
What the Guidelines Say-And What Doctors Ignore
The American Urological Association (AUA) has been clear since 2022: Do not prescribe anticholinergics to anyone with a history of urinary retention or significant bladder outlet obstruction. The FDA requires black box warnings on all anticholinergic labels for this exact reason. The European Medicines Agency banned their use in patients with prior retention in 2021. Yet, these warnings are still ignored. Why? Because many doctors still see anticholinergics as “first-line” for overactive bladder. They’re cheap. They’re familiar. They’re in every pharmacy. Dr. Jerry G. Blaivas, a top urologist at Albert Einstein College of Medicine, says bluntly: “Anticholinergics should be considered absolutely contraindicated in men with a history of urinary retention or significant prostate enlargement.” But not all experts agree. Dr. Victor Nitti argues low doses can be safe with careful monitoring. The problem? Monitoring is rare. Only 1 in 4 patients get a baseline post-void residual (PVR) test before starting these drugs.What You Need to Do Before Taking These Drugs
If you’re being prescribed an anticholinergic for overactive bladder, here’s what you must ask for:- Baseline PVR test-a bladder scan that measures how much urine is left after you pee. If it’s over 100 mL, you’re already at risk. Over 150 mL? Don’t take the drug.
- Prostate check-even if you think you’re fine. A simple ultrasound can show if your prostate is enlarged.
- ACB score review-ask your pharmacist or doctor to add up all your meds. If your total is 3 or higher, consider alternatives.
- Start low, go slow-if you must take it, begin with 25% of the dose and wait two weeks. Check your PVR again.
Alternatives That Actually Work-Without the Risk
You don’t have to suffer from overactive bladder. And you don’t have to risk retention. - Mirabegron (Myrbetriq): Works by relaxing the bladder muscle through a different pathway (beta-3 receptors). Retention risk? Just 0.3%. That’s 5 times lower than anticholinergics. It’s now the first-line choice for men in Europe and increasingly in the U.S. - OnabotulinumtoxinA (Botox injections into the bladder): Reduces urgency and frequency. Retention risk? Only 0.5%. Requires a specialist, but it’s safe and lasts 6-9 months. - Peripheral neuromodulation (PTNS or InterStim): Uses mild electrical pulses to retrain bladder nerves. No drugs. No catheters. Proven effective for overactive bladder. - Lifestyle changes: Cut caffeine, limit fluids before bed, pelvic floor exercises. These help more than you think. Market data shows the shift is already happening. In 2015, anticholinergics made up 58% of overactive bladder prescriptions. By 2022, that dropped to 40%. Mirabegron now holds 31% of the market. Doctors are catching on.
Real Stories: What Happens When You Don’t Ask Questions
On Drugs.com, user JohnM72 wrote: “After two weeks of oxybutynin 5mg, I couldn’t pee at all. Ended up in the ER with a catheter. My urologist said, ‘This happens in 1 out of 50 men your age.’ I didn’t know I was one of them.” Reddit’s r/urology has over 127 posts since 2020 about anticholinergic-induced retention. The top thread? A 71-year-old man who went to the ER after taking tolterodine. He’d been told it was “safe.” He wasn’t scanned. He wasn’t warned. But there’s hope. CathyR on HealthUnlocked shared: “My urologist checks my PVR every month. I’ve been on solifenacin 5mg for 18 months without issues-because we caught my residual rising to 150mL and cut my dose. I’m still dry, and I still pee.”What to Do If You’re Already on an Anticholinergic
If you’re taking one of these drugs right now:- Check if you’ve ever had a bladder scan. If not, ask for one.
- Watch for warning signs: Straining to start urinating, weak stream, feeling like you haven’t emptied, needing to push or bear down.
- If you can’t pee for more than 12 hours-go to urgent care. Don’t wait. Catheterization is a simple fix, but the longer you wait, the more damage you risk.
- Ask your doctor about switching to mirabegron or another alternative.
The Bottom Line
Anticholinergics aren’t evil drugs. They help people. But they’re not safe for everyone-and too many doctors treat them like harmless pills. If you’re a man over 65, or have any prostate issues, or take multiple medications, you’re not just at risk-you’re in the danger zone. The science is clear. The guidelines are clear. The real-world stories are clear. Don’t let a routine prescription turn into a medical emergency. Ask for a bladder scan. Ask about alternatives. Ask before you swallow.Your bladder can’t speak up. You have to speak for it.

Comments
Okay, so let me get this straight: we’re prescribing M3 receptor antagonists to geriatric males with BPH-despite the FDA’s black box warning-and then acting shocked when they can’t void? The pharmacokinetics are clear, the clinical data is robust, and yet, we’re still treating this like a ‘trial-and-error’ scenario. This isn’t medical practice; it’s negligence dressed up as protocol. The ACB scale isn’t optional-it’s a lifeline. If your patient’s cumulative score hits 3+, you’re not managing a condition-you’re manufacturing a urological emergency.
So let me summarize: doctors give pills that turn bladders into concrete blocks, then act surprised when patients end up in the ER with a catheter. And the worst part? They act like it’s the patient’s fault for not ‘asking questions.’ Newsflash: most people don’t know what ‘M3 receptors’ are. They trust their doctor. That’s the contract. Break it, and you’re not a healer-you’re a hazard.
Of course this is happening. The FDA, the AMA, the WHO-they’re all in bed with Big Pharma. These drugs are pushed because they’re profitable. Mirabegron? Too expensive. Botox? Too ‘experimental.’ Meanwhile, old men are getting catheterized because some pharma rep convinced a doctor that oxybutynin is ‘safe.’ Wake up. This isn’t medicine-it’s corporate control disguised as healthcare.
I had my dad on oxybutynin. One week later-catheter. No warning. No scan. Just ‘take this.’ Now he’s on mirabegron. No issues. Why isn’t this common knowledge? Why are we still doing this?
It is both regrettable and lamentable that the clinical imperative to preserve urinary function has been systematically subordinated to the commercial imperatives of pharmaceutical marketing. The persistence of anticholinergic prescribing in populations with documented anatomical predisposition to outlet obstruction constitutes a profound failure of clinical governance, evidence-based medicine, and professional ethics. The fact that baseline PVR measurement is performed in fewer than 25% of cases is not merely an oversight-it is an institutionalized dereliction of duty. One must ask: if a medication carries a black box warning, why is it still considered first-line? The answer, regrettably, lies not in science, but in inertia, ignorance, and institutional complacency.
Interesting how everyone’s suddenly concerned about urinary retention… but no one’s talking about the fact that mirabegron is just a beta-3 agonist repackaged as ‘innovative’-when it was originally developed for cardiovascular applications. And don’t get me started on the ‘lifestyle changes’ crowd-pelvic floor exercises? Really? That’s your solution for a neurogenic bladder? This entire discourse is performative medicine-everyone wants to sound woke, but nobody wants to fund proper urodynamic studies.
bro i took oxybutynin for 3 days and i couldnt pee at all… my roomate had to call 911… the er doc was like ‘oh yeah this happens’ and i was like… wait… you knew this? why didnt you tell me?? now im scared to take any med… even tylenol
While the empirical evidence presented is both statistically significant and clinically relevant, it is imperative to acknowledge the broader systemic context: the fragmentation of primary care in the United States, the erosion of continuity of care, and the institutional disincentives against time-intensive diagnostic protocols such as post-void residual measurement. The physician, operating under time constraints imposed by managed care, is not inherently negligent-rather, he is a cog in a machine designed to prioritize throughput over safety. The solution, therefore, cannot lie in blaming individual practitioners, but in restructuring reimbursement models to incentivize preventive urological assessment.
Let me tell you something about the West and its obsession with pills. In India, we’ve known for centuries that the body is not a machine to be fixed with chemicals-it’s a flow, a rhythm. We use herbs, diet, yoga, breathing. But no, you want a pill that stops your bladder from working because it’s easier than changing your coffee habit. You call this progress? This is cultural arrogance disguised as science. You have 127 Reddit threads about catheters because you refuse to look at the root: your lifestyle, your diet, your stress. You don’t need a new drug-you need to stop treating your body like a broken iPhone.