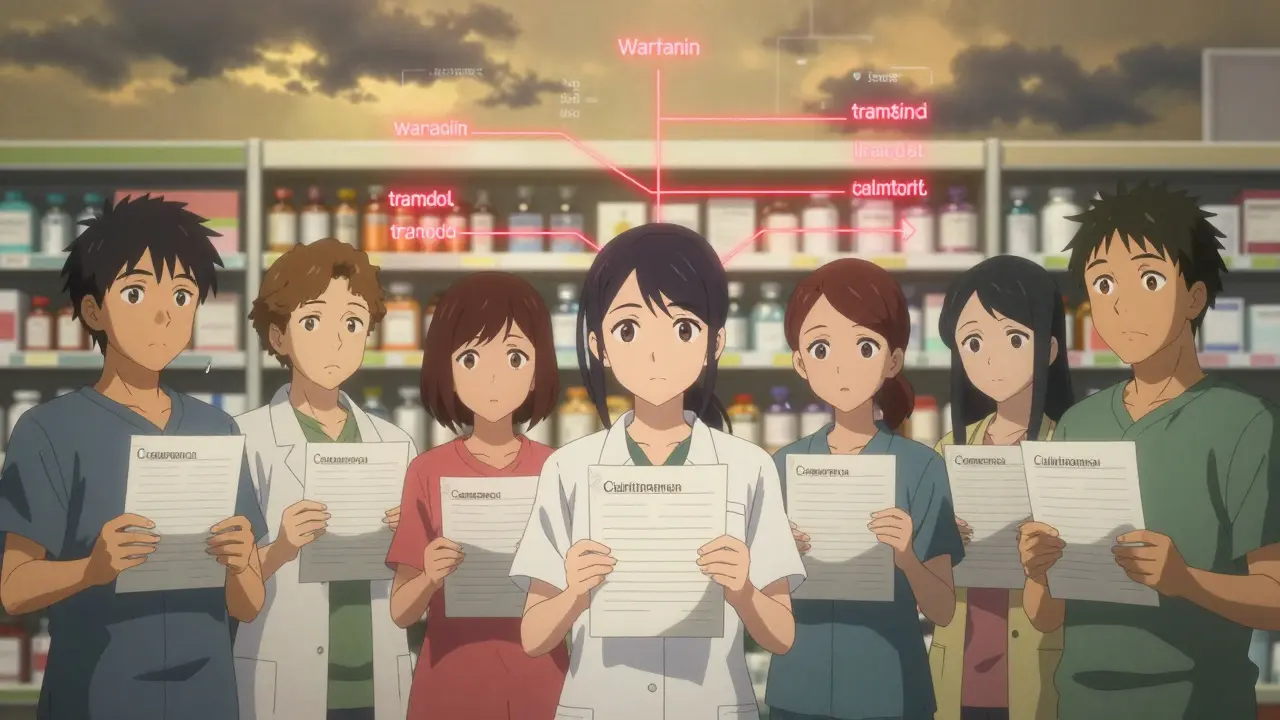
Drug Interaction Checker
Enter medications you're currently taking. This tool checks for dangerous interactions based on the latest medical research.
This tool identifies potentially dangerous combinations based on the article content and medical research:
- Checks for dangerous interactions between commonly prescribed medications
- Highlights critical risks with severity levels
- Provides information on why certain combinations are problematic
When you take more than one medication, something invisible is happening inside your body. Two drugs might be working against each other, or one could be forcing the other to build up to dangerous levels. This isn’t rare. In fact, drug interactions are behind a huge number of hospital visits and emergency trips - and most of them are completely avoidable.
What Exactly Is a Drug Interaction?
A drug interaction happens when one substance changes how another drug works in your body. It’s not just about pills. It can be food, supplements, even grapefruit juice. The result? Side effects that get worse, last longer, or show up when they shouldn’t.Think of your body like a factory. Drugs are workers. Some help clean up, others deliver supplies. But if two workers start interfering with each other’s tools, chaos happens. One might slow down the cleanup crew. Another might overload the system. That’s when side effects go from mild to serious.
There are two main ways this happens. The first is pharmacokinetic - how your body absorbs, breaks down, or gets rid of the drug. The second is pharmacodynamic - how the drugs act on your cells when they meet. Both can turn a safe dose into a dangerous one.
The Hidden Culprit: CYP3A4
If you’ve ever heard of CYP3A4, it’s because this enzyme is the most important player in drug interactions. It’s responsible for breaking down about half of all medications you take. When something blocks or overloads this enzyme, drugs pile up like traffic on a highway.Common blockers? Antibiotics like clarithromycin, antifungals like ketoconazole, and even grapefruit juice. Take statins (cholesterol drugs) with one of these, and your risk of muscle damage jumps 8.4 times. That’s not a guess - it’s from a 2013 study in the New England Journal of Medicine. One patient got rhabdomyolysis. Another ended up in the ICU.
And it’s not just antibiotics. Antivirals, heart meds, even some cancer drugs can be affected. The FDA says CYP3A4 is involved in 63% of all serious drug interactions. That’s not a small risk. It’s the biggest single factor in preventable harm.
Warfarin and the Silent Danger
Warfarin is a blood thinner. It’s prescribed to millions. But it’s also one of the most dangerous drugs when combined with other substances.Take aspirin. It thins blood too. Together, they can increase bleeding risk by 70-100%. That’s not just nosebleeds. It’s internal bleeding, strokes, even death.
What about acetaminophen? You’d think it’s harmless. But take more than 2 grams a day - just six regular painkillers - and your warfarin levels spike. A 2015 study in JAMA Internal Medicine found this combo raised bleeding risk by 1.8 times. Most patients didn’t even know.
And then there’s vitamin K. Found in spinach, kale, broccoli. It reverses warfarin’s effect. Eat a big salad one day, skip it the next, and your INR (a blood test that measures clotting) goes wild. One patient I read about had three hospital stays in six months just because her diet changed.

Genetics: Why It Hits Some Harder
You might be wondering why two people take the same drugs, same doses, but only one gets sick. The answer? Genetics.Three to ten percent of white people lack a working version of CYP2D6, the enzyme that turns codeine into morphine. For them, codeine does nothing. For others? It turns into too much morphine. That’s why some people get extreme drowsiness or breathing trouble after a single dose.
The FDA says 30% of commonly prescribed drugs have genetic risks tied to them. That includes antidepressants, beta-blockers, and even some ADHD meds. Yet, most doctors don’t test for it. Why? Cost, time, lack of awareness. But the data is clear: if you’re a poor metabolizer, your side effects aren’t random. They’re predictable.
Polypharmacy: The Perfect Storm
Taking five or more medications? You’re in high-risk territory. A 2024 study of 563 patients found that people on five or more drugs had a 78% higher chance of a bad reaction. With ten or more? That number jumps to 153%.Why? More drugs = more chances for collisions. Common dangerous combos:
- SSRIs (like fluoxetine) + tramadol → serotonin syndrome (seizures, fever, confusion)
- Amiodarone + furosemide → dangerous drops in potassium → heart rhythm issues
- Clarithromycin + prednisolone → increased stomach bleeding risk
These aren’t theoretical. The Hughes study documented 21 cases of warfarin-aspirin bleeding, 7 cases of clarithromycin-prednisolone bleeding, and 6 cases of amiodarone-furosemide heart problems. All happened in real patients. All were preventable.
What Patients Are Saying
Look at Reddit threads from r/pharmacy in late 2023. Over 140 patients shared stories:- “Took simvastatin with grapefruit juice. Couldn’t walk for weeks. Muscle pain so bad I needed a wheelchair.”
- “My doctor didn’t warn me about sertraline and tramadol. I had a seizure.”
- “I took omeprazole with clopidogrel. My heart attack risk went up. No one told me.”
On Drugs.com, medications with high interaction potential get ratings 1.2 stars lower than similar drugs. The most common complaint? “I wasn’t warned.”
How to Protect Yourself
The good news? Most of this is preventable. Here’s how:- Keep a full list - every pill, supplement, herbal tea, OTC painkiller. Bring it to every appointment.
- Ask your pharmacist - they’re trained to spot interactions. Most hospitals have them on staff. Use them.
- Know your high-risk drugs - anticoagulants, antiarrhythmics, antidepressants, and statins are the top offenders.
- Check grapefruit - if your drug has a warning, avoid it entirely. No exceptions.
- Use one pharmacy - it lets them track everything you’re taking in one system.
One study showed that patients who used a single pharmacy had 30% fewer interaction-related hospital visits. That’s not magic. It’s systems working.
What Doctors Are Missing
A 2023 survey of 3,500 doctors found 74% felt overwhelmed by interaction alerts. 58% admitted they sometimes ignored them. Why? Alert fatigue.Electronic health records flood doctors with warnings - 90-95% of which are low-risk. “Take ibuprofen with your blood pressure pill” - okay, maybe. But “don’t take clarithromycin with simvastatin” - that’s a red flag. Right now, the system screams too much. And we stop listening.
Some hospitals are fixing this. Tiered alerts - only the high-risk ones pop up. Others use pharmacists to review complex cases. The results? A 45% drop in dangerous interactions. It works. But it’s not everywhere.
The Future: AI and Personalized Medicine
New tools are coming. AI models now predict dangerous combos with 89% accuracy - better than older systems. The NIH is testing pharmacogenetic testing in 15 health systems. Early results? A 36% drop in high-risk interactions.Wearable sensors are being tested to track how fast your body processes drugs in real time. Imagine a patch that tells your doctor, “Your warfarin level is rising - adjust dose now.” That’s not sci-fi. It’s in Phase 2 trials.
But none of this matters if we don’t change how we talk about meds. You need to know your drugs. Your doctor needs to listen. And the system needs to stop drowning us in noise.
Can over-the-counter drugs cause dangerous interactions?
Absolutely. Even simple painkillers like ibuprofen or naproxen can interfere with blood pressure meds, increasing kidney strain or raising blood pressure. Antihistamines like diphenhydramine (Benadryl) can worsen confusion in older adults or interact with antidepressants. Herbal supplements like St. John’s Wort can make birth control, antidepressants, or transplant drugs fail. There’s no such thing as a "safe" OTC drug when you’re on multiple prescriptions.
Is grapefruit juice really that dangerous?
Yes, for certain drugs. Grapefruit juice blocks CYP3A4 in the gut, which can cause drugs like simvastatin, felodipine, or cyclosporine to build up to 3-5 times their normal level. One small glass can last 24 hours. Even if you take your pill at night and juice in the morning, it still counts. If your drug label says "avoid grapefruit," skip it. No exceptions. Amlodipine and lisinopril are safe - but if you’re unsure, ask your pharmacist.
Why don’t doctors always warn me about interactions?
It’s not laziness - it’s overload. Doctors see dozens of patients a day. There are over 1,000 known drug interactions. EHR systems bombard them with alerts, 90% of which are low-risk. Many stop trusting the system. Plus, not all doctors get updated training on interactions. If you’re on five or more drugs, ask specifically: "Could any of these interact?" Don’t wait for them to bring it up.
Do supplements count as drugs in interactions?
Yes, and they’re often the hidden cause. St. John’s Wort can make birth control, antidepressants, and blood thinners fail. Vitamin K can undo warfarin. Magnesium can reduce antibiotic absorption. Omega-3s can increase bleeding risk with anticoagulants. Just because it’s "natural" doesn’t mean it’s safe. Always list every supplement - even ones you only take once a week.
What should I do if I think I’m having an interaction?
Don’t stop your meds on your own. Call your pharmacist or doctor immediately. Write down what you took, when, and what symptoms you’re feeling - muscle pain, dizziness, confusion, unusual bleeding, or irregular heartbeat. These are red flags. If it’s severe (chest pain, trouble breathing, fainting), go to the ER. Bring your full med list. Most ER staff won’t know your history - your list is your best tool.
If you’re on multiple medications, you’re not alone. But you don’t have to accept the risk. Knowledge is your shield. Ask questions. Keep lists. Use your pharmacist. And never assume a drug is safe just because it’s common. Your body is a system - and every pill you take changes how the whole thing runs.

Comments
Man, this post is a wake-up call. I never realized how many of my meds could be quietly sabotaging each other. I’m on three prescriptions and a turmeric supplement-now I’m terrified. But seriously, thank you for laying this out so clearly. I’m scheduling a pharmacy consult tomorrow. Knowledge is power, folks.
...and nobody’s talking about the pharmaceutical companies?!! They KNOW this happens. They design drugs to be dependent on each other-so you keep buying more. Grapefruit juice? That’s just the tip of the iceberg. The real villain? The FDA’s approval process. They’re in bed with Big Pharma. I’ve seen the documents. It’s not an accident-it’s a business model.
Oh, so now we’re blaming grapefruit juice? Classic. Let me guess-the next thing you’ll say is that vaccines cause autism? Look, I’ve been on statins for 12 years with grapefruit juice every morning. No issues. My doctor laughs at this fear-mongering. This whole post reads like a TikTok scare tactic. If you’re scared of your meds, stop taking them. Don’t let some blog post make you paranoid.
Let’s be real-this isn’t about drug interactions. It’s about how broken our healthcare system is. Doctors get 8 minutes per patient. Pharmacists? Underpaid and ignored. EHRs scream like a broken fire alarm. And we wonder why people end up in the ER? It’s not that the science is unclear-it’s that the system is designed to fail you. I’ve seen patients die because their cardiologist didn’t check their supplements. And no one gets fired for it. That’s the real horror story.
soooo i just found out my omeprazole messes with clopidogrel?? omg i’ve been taking both for 3 years 😭 i thought omeprazole was just for heartburn… i’m calling my doc right now. also, why does no one tell you this stuff??
I took sertraline and tramadol for 6 months. Didn’t know it was a thing. Got dizzy, nauseous, felt like I was floating. Thought I was just stressed. Turns out? Serotonin syndrome. Scary stuff. My pharmacist caught it during a refill. She saved me. Use your pharmacist. They’re the unsung heroes.
Let me tell you about my cousin. She was on warfarin. Ate kale smoothies every morning. INR went from 2.8 to 0.9 in three days. Ended up with a pulmonary embolism. Then she stopped the kale, started eating McDonald’s again-INR stabilized. Who knew broccoli was a silent killer? This isn’t medicine. It’s a minefield. And we’re all just walking through it blindfolded.
AI-driven pharmacogenomics is the future. We’re already seeing hospitals reduce adverse events by 36% with genetic screening. This isn’t sci-fi-it’s happening now. The real question: Why aren’t we mandating this for patients on 5+ meds? It’s cheaper than ICU stays. And yet… we still treat it like a luxury. We’re so backwards. We need policy change, not just awareness.
Thank you for writing this. Seriously. I’m a nurse, and I see this every day. Patients think ‘natural’ means safe. St. John’s Wort with antidepressants? Dangerous. Turmeric with blood thinners? Big no. We need more education-not just for patients, but for doctors too. Let’s normalize asking, ‘What else are you taking?’ at every visit. It’s simple. It’s vital. And it saves lives.
My grandma takes 11 meds. I help her manage them. We use one pharmacy, keep a printed list, and she texts me every time she starts something new-even a new cough syrup. It’s not glamorous. But it’s working. She’s been hospital-free for 18 months. This isn’t rocket science. It’s consistency. And love. You can do this too.
India has 700 million elderly people on polypharmacy and zero pharmacist access. We have a crisis. But you Americans? You have the tech, the data, the resources-and you’re still letting people die because your EHRs are broken? I’m ashamed. This isn’t just a medical issue. It’s a moral one. We need global reform. Not just blog posts. Real action.
Did you know that 72% of drug interaction deaths happen in people over 65? And yet, no one talks about it. I’ve been silent about my meds for years. I didn’t want to seem ‘difficult.’ But now? I’m not silent anymore. I carry my list. I ask questions. I’m done being polite about my life.
So… grapefruit juice blocks CYP3A4. Got it. But what about orange juice? Or apple juice? Or… tea? I read a study once that said green tea might interfere with beta-blockers. Is everything dangerous now? I’m starting to think the only safe thing is to stop taking all meds and eat only raw kale. (I’m joking. Kind of.)
Wow. This post reads like a 2012 Reddit thread that got accidentally uploaded to WebMD. ‘Grapefruit juice bad’? Shocking. ‘Doctors overwhelmed’? Revolutionary. Next up: ‘Water can be dangerous if you drink too much.’ This isn’t news. It’s just a rehash with fancy graphs. I’ve been on 8 meds for 8 years. Still breathing. Still walking. Still not scared of my supplements.
I’ve been on warfarin for 10 years. I eat spinach. I take vitamin D. I drink grapefruit juice. My INR is stable. I get tested weekly. I have a good pharmacist. It’s not magic. It’s routine. Don’t panic. Just stay informed. And talk to someone who knows.