Caffeine Medication Interaction Checker
Check Your Medication Interactions
Select your medication and your caffeine intake to see potential interactions and safety guidelines.
Interaction Results
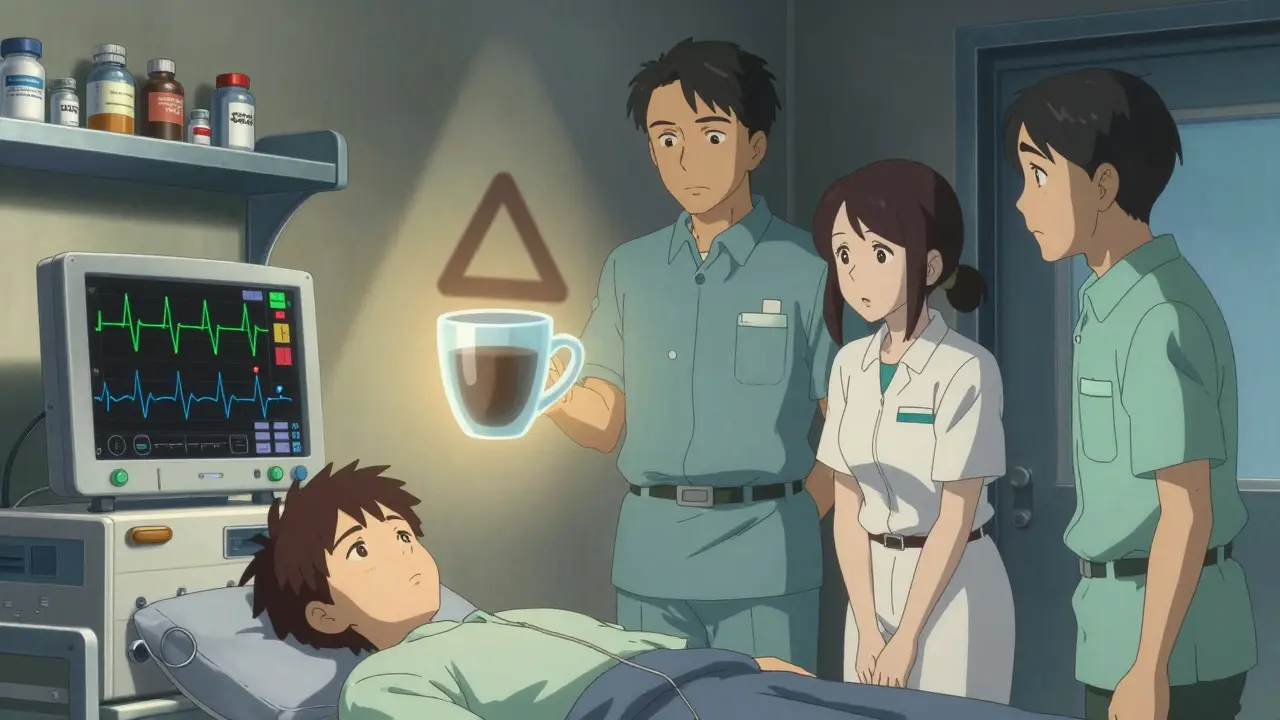
Many people start their day with a cup of coffee, unaware that it might be quietly undermining their medication. Caffeine isn’t just a pick-me-up-it’s a powerful chemical that interacts with dozens of common drugs, sometimes making them less effective or dangerously strong. These aren’t rare edge cases. Caffeine medication interactions are behind thousands of avoidable hospital visits every year, especially in older adults who take multiple prescriptions.
How Caffeine Changes How Your Body Handles Medicines
Caffeine doesn’t just buzz through your system. It actively interferes with how your liver breaks down drugs. The key player here is an enzyme called CYP1A2. About 10-15% of all prescription medications rely on this enzyme to be processed and cleared from your body. Caffeine blocks it-like jamming a lock. That means drugs stick around longer than they should, building up to unsafe levels.
But it’s not just about liver enzymes. Caffeine also acts like a fake key for certain receptors in your brain and heart. It blocks adenosine, a natural calming signal. That’s why you feel alert. But when you’re taking heart medications like adenosine or dipyridamole, caffeine essentially cancels them out. That’s why you’re told to avoid coffee for 24 hours before a stress test-your heart won’t respond properly if caffeine is still in your system.
Thyroid Medication: Coffee Can Make Your Pill Work Less
If you take levothyroxine (Synthroid, Levoxyl, or generic), drinking coffee right after taking your pill can slash its absorption by up to 57%. That’s not a small drop-it’s enough to push your TSH levels out of range. One patient shared on a thyroid forum: “I’d been stable for years, then my TSH jumped from 1.8 to 4.5. Turns out, I was drinking coffee 10 minutes after my pill.”
The fix? Wait 30 to 60 minutes after taking your thyroid medication before having coffee. It’s simple, but most people don’t know. Even decaf coffee contains 2-15 mg of caffeine-enough to interfere if you’re sensitive. The Endocrine Society made this timing official in 2019. Stick to it.
Warfarin and Other Blood Thinners: A Dangerous Combo
Warfarin (Coumadin) is one of the most dangerous drugs to mix with caffeine. Caffeine slows down how fast your body clears warfarin, causing your INR-a measure of how long your blood takes to clot-to rise by 15-25% within a day. That means you’re at higher risk of bleeding, even from minor cuts or bruises.
The American Heart Association says if you’re on warfarin, limit caffeine to no more than 200 mg a day (about two cups of coffee) and keep your intake consistent. Skipping coffee one day and drinking three the next causes wild INR swings. That’s why emergency rooms see so many cases where patients think they’re fine until they start bleeding internally.
Antidepressants: Coffee Can Make You More Anxious-or Less Helped
Antidepressants react differently to caffeine. Some, like fluvoxamine (Luvox), get blocked by caffeine, reducing absorption by 33%. That means you’re not getting the full dose. Others, like amitriptyline, get stuck in your system because caffeine shuts down the liver enzyme that clears them. Plasma levels can jump 20-40%, leading to dizziness, dry mouth, heart palpitations, and worse.
Patients on SSRIs often report feeling more jittery, anxious, or unable to sleep after adding coffee. A Drugs.com review of 1,247 users found 68% said their anxiety got worse when they drank coffee with their meds. Harvard Health warns: “Drinking coffee with fluvoxamine or escitalopram can turn a manageable dose into an overdose.”
Heart Medications: Caffeine Can Raise Your Blood Pressure-and Your Risk
If you’re on blood pressure meds like verapamil, caffeine can blunt their effect. Mayo Clinic notes that within 2-3 hours of coffee, diastolic blood pressure can rise by 8-12 mmHg. That’s enough to undo weeks of controlled treatment.
Even worse, caffeine combined with stimulants like pseudoephedrine (found in cold meds) can spike heart rate by 20-35 beats per minute and systolic blood pressure by 15-25 mmHg within 45 minutes. That’s a recipe for arrhythmia or even heart attack in vulnerable people. University Hospitals flagged this in their June 2025 update, especially for those with existing heart conditions.
Seizure Medications: Caffeine Can Trigger Seizures
If you have epilepsy and take carbamazepine, phenytoin, valproate, or other seizure drugs, caffeine can lower their effectiveness. A 2019 study in Epilepsy & Behavior found patients who drank regular coffee had 18-35% more seizures than those who avoided it. Caffeine lowers the seizure threshold-it makes your brain more excitable.
It’s not just about quantity. One cup of coffee a day can be enough to cause problems in sensitive individuals. Doctors now routinely ask patients with epilepsy about caffeine intake. If you’re struggling with breakthrough seizures, cutting coffee might be the missing piece.
ADHD Medications: Double the Stimulant, Double the Risk
Adderall, Ritalin, and other stimulants already speed up your heart and nervous system. Add caffeine, and you’re stacking fuel on fire. Patients on PatientsLikeMe describe feeling “shaky, wired, and unable to sleep for 12 hours.” Heart rates can hit 120+ bpm. Some report panic attacks or chest tightness.
There’s no safe threshold here. Even one cup of coffee with your morning Adderall can push you into dangerous territory. The safest move? Avoid caffeine entirely while on stimulants. If you must have coffee, wait at least 4 hours after your dose.

Diabetes and Cold Medicines: A Hidden Danger
Many people don’t realize that decongestants like pseudoephedrine often come with caffeine in combo products. For diabetics, this combo is a triple threat: caffeine raises blood sugar, pseudoephedrine raises it more, and both can spike body temperature by 0.5-1.0°C. University Hospitals found blood sugar spikes of 15-25 mg/dL in diabetic patients who took these combo meds with coffee.
Check labels. If a cold medicine says “PM” or “Day & Night,” it might contain caffeine. Even “non-drowsy” formulas can have it. If you have diabetes, avoid caffeine-containing cold meds entirely. Use plain pseudoephedrine or a caffeine-free alternative.
What You Can Do: Simple Rules to Stay Safe
- Wait at least 30-60 minutes after taking thyroid medication before drinking coffee.
- Avoid caffeine for 24 hours before a cardiac stress test.
- Limit coffee to 2 cups per day if you’re on warfarin-and keep your intake the same every day.
- Don’t mix caffeine with stimulant ADHD meds. Wait 4+ hours after your dose if you must have it.
- Check cold and allergy meds for caffeine. Choose caffeine-free versions.
- Decaf isn’t caffeine-free. It still has 2-15 mg per cup-enough to interfere with sensitive drugs.
- Ask your pharmacist: “Does my medication interact with caffeine?” Don’t assume it’s safe.
When to Call for Help
Some caffeine-medication reactions are emergencies. Seek immediate medical care if you experience:
- Heart rate over 120 bpm or irregular heartbeat
- Systolic blood pressure above 180 mmHg
- Difficulty breathing or chest pain
- Confusion, vision changes, or loss of coordination
- Twitching, rigid muscles, or tremors
- Seizures or altered mental state
- Suicidal thoughts or worsening depression
These aren’t normal side effects. They’re red flags that your body is overwhelmed by the combo of caffeine and your medication.
Why This Keeps Happening
Doctors don’t always ask about coffee. Patients don’t realize caffeine is in tea, energy drinks, chocolate, and even some pain relievers. The American Pharmacists Association says caffeine-medication interactions cause 2.8% of all adverse drug events in adults-rising to 4.2% in those over 65. That’s tens of thousands of preventable hospital visits every year.
Thankfully, things are changing. Drug databases like Micromedex now warn about caffeine interactions for 127 medications-up from 89 in 2020. The FDA now requires caffeine warnings on 15 new drug labels. Most major hospitals have added caffeine screening to their electronic health records.
But the biggest barrier isn’t technology-it’s awareness. You’re not alone if you didn’t know this. But now that you do, you can protect yourself. Talk to your pharmacist. Read your labels. Adjust your routine. Your meds-and your health-depend on it.
Can I drink coffee while taking antidepressants?
It depends on the medication. Coffee can reduce the effectiveness of fluvoxamine and escitalopram by up to 33%. For amitriptyline and other tricyclics, it can increase blood levels by 20-40%, raising the risk of side effects like dizziness, dry mouth, or heart palpitations. If you take antidepressants, talk to your doctor or pharmacist before drinking coffee. Many patients find switching to decaf or cutting back helps reduce anxiety and sleep problems.
Does decaf coffee affect medications?
Yes. Decaf coffee still contains 2-15 mg of caffeine per cup. For most people, that’s not a problem. But if you’re taking thyroid medication, seizure drugs, or certain antidepressants, even small amounts can interfere. If you’re sensitive or on a medication with narrow therapeutic windows, treat decaf like regular coffee-wait 30-60 minutes after taking your pill before drinking it.
How long should I wait after taking medicine before drinking coffee?
It varies by drug. For levothyroxine, wait 30-60 minutes. For blood thinners like warfarin, consistency matters more than timing-stick to the same amount daily. For stimulant ADHD meds, wait at least 4 hours. For cardiac stress tests, avoid caffeine for 24 hours. When in doubt, wait 2 hours after taking your pill before drinking coffee. Always check with your pharmacist for your specific medication.
Can caffeine make my blood pressure medication less effective?
Yes. Caffeine can temporarily block the effect of blood pressure drugs like verapamil, causing diastolic pressure to rise by 8-12 mmHg for 2-3 hours. It’s not permanent, but if you drink coffee daily, your blood pressure may stay higher than it should. If you’re on blood pressure meds, try cutting back or switching to decaf. Monitor your numbers for a week to see if it helps.
What cold medicines contain caffeine?
Many “non-drowsy” or “daytime” cold and flu remedies contain caffeine to counteract drowsiness from antihistamines. Common examples include Excedrin, Midol Complete, and some versions of DayQuil and NyQuil. Always check the “Active Ingredients” list on the label. If you see “caffeine” listed, avoid it if you’re on heart, thyroid, or diabetes meds. Choose caffeine-free alternatives like plain pseudoephedrine or guaifenesin.


Comments
Let’s be real-most people treat caffeine like a harmless ritual, but this post lays bare the terrifying biochemical warfare happening in their bodies every morning. CYP1A2 isn’t some abstract enzyme-it’s the bouncer at the liver’s nightclub, and caffeine just kicked it out and brought in a whole crew of uninvited drugs. The fact that 57% absorption drop for levothyroxine isn’t common knowledge is a scandal. If your endocrinologist didn’t tell you this, they’re not doing their job. This isn’t ‘coffee etiquette’-it’s pharmacological survival.
Wow, I had no idea decaf was still a problem. I’ve been sipping my ‘decaf’ latte 5 minutes after my Synthroid like a champ. Guess I’m just lucky I haven’t turned into a zombie yet. Thanks for the wake-up call-literally. Also, anyone else feel like the FDA’s just catching up to what pharmacists have known since 1998?
Bro this is life changing. I take Adderall and coffee like it’s breakfast and lunch. Now I know why I was shaking like a leaf and couldn’t sleep for 2 days. Going decaf from now. No more caffeine after 12pm. My heart will thank me 😊
It is, indeed, a matter of profound public health significance that the average consumer remains blissfully unaware of the pharmacokinetic implications of habitual caffeine consumption in conjunction with prescribed therapeutics. The data presented here, meticulously sourced and clinically validated, ought to be disseminated via primary care screening protocols and pharmacy counseling mandates. One might even argue for mandatory labeling on all caffeinated products, akin to tobacco warnings.
Look, I get it-coffee is a sacrament for the overworked, the sleep-deprived, the corporate serfs. But let’s not pretend this is some kind of revelation. The interactions between caffeine and medications have been documented since the 1970s. The real problem? The medical-industrial complex doesn’t want you to know this stuff because if you did, you’d stop taking half your prescriptions and start drinking green tea and doing yoga. And who profits from that? Big Pharma, obviously. They’ve been quietly funding studies that downplay caffeine’s role for decades. The fact that you’re only now hearing about this? That’s not ignorance-it’s systemic suppression.
They don’t want you to know this because the FDA, WHO, and Big Pharma are all in bed with the coffee cartel. Caffeine is a controlled substance disguised as a beverage. The real reason they don’t warn you? It’s because if people stopped drinking coffee, the entire economy of ‘productivity culture’ would collapse. And don’t get me started on how decaf is laced with chemical solvents that mess with your mitochondria. This isn’t just about drug interactions-it’s about chemical enslavement. Wake up. The coffee is poisoned. The system is rigged. And they’re watching you sip it.
Thank you for this comprehensive overview. However, I must point out a minor typographical error on page 4: ‘slashed its absorption’ should be ‘slashes its absorption’ for grammatical accuracy. Additionally, the reference to ‘University Hospitals June 2025 update’ appears to be anachronistic, as we are currently in 2024. Please revise accordingly for scholarly integrity.
I’ve been on warfarin for 8 years and never knew my coffee habit could mess with my INR. I’ve been drinking 2 cups a day, every day, no changes. Maybe that’s why my numbers have been so stable. I’ll keep doing what I’m doing-but now I know why. Thanks for the clarity. Also, decaf is still coffee to me. I’ll just sip it slower now.
As someone who’s spent 15 years as a pharmacist, I’ve seen this play out too many times. A patient comes in with a spike in INR, and we find out they had a ‘special’ coffee at the weekend. Or they suddenly stopped drinking coffee and their antidepressant side effects vanished. It’s not magic-it’s pharmacology. The sad part? Most GPs still don’t ask about caffeine. We need better training. And patients need to feel safe bringing it up. This post? It’s a step in the right direction.
Just got back from my endo appointment and I’m crying because I’ve been drinking coffee 5 mins after my thyroid med for 3 years. My TSH was 5.2. Now I know why. I switched to water and waiting an hour. I feel like an idiot but also so much more in control. Thank you for writing this. I’m sharing it with my mom who’s on 7 meds.
I just stopped coffee for a week and my anxiety went from 8/10 to 2/10. I didn’t even realize it was the coffee.