Tacrolimus Neurotoxicity Risk Assessment Tool
This tool helps you assess your risk of developing neurotoxicity symptoms while taking tacrolimus. Your results will be based on key factors that influence risk, including your transplant type, blood levels, medications, and genetics.
When you’ve just had a transplant, the last thing you want is to feel like your body is betraying you. You’re taking tacrolimus to keep your new organ alive, but now your hands won’t stop shaking. Your head pounds like it’s under a vice. You can’t sleep. You’re not imagining it - this is tacrolimus neurotoxicity, and it’s more common than most doctors let on.
What Tacrolimus Neurotoxicity Actually Feels Like
Tacrolimus is one of the most powerful immunosuppressants used after kidney, liver, heart, or lung transplants. It works by shutting down the immune system’s attack on your new organ. But it doesn’t know the difference between a threat to your transplant and normal brain activity. That’s where things go wrong.
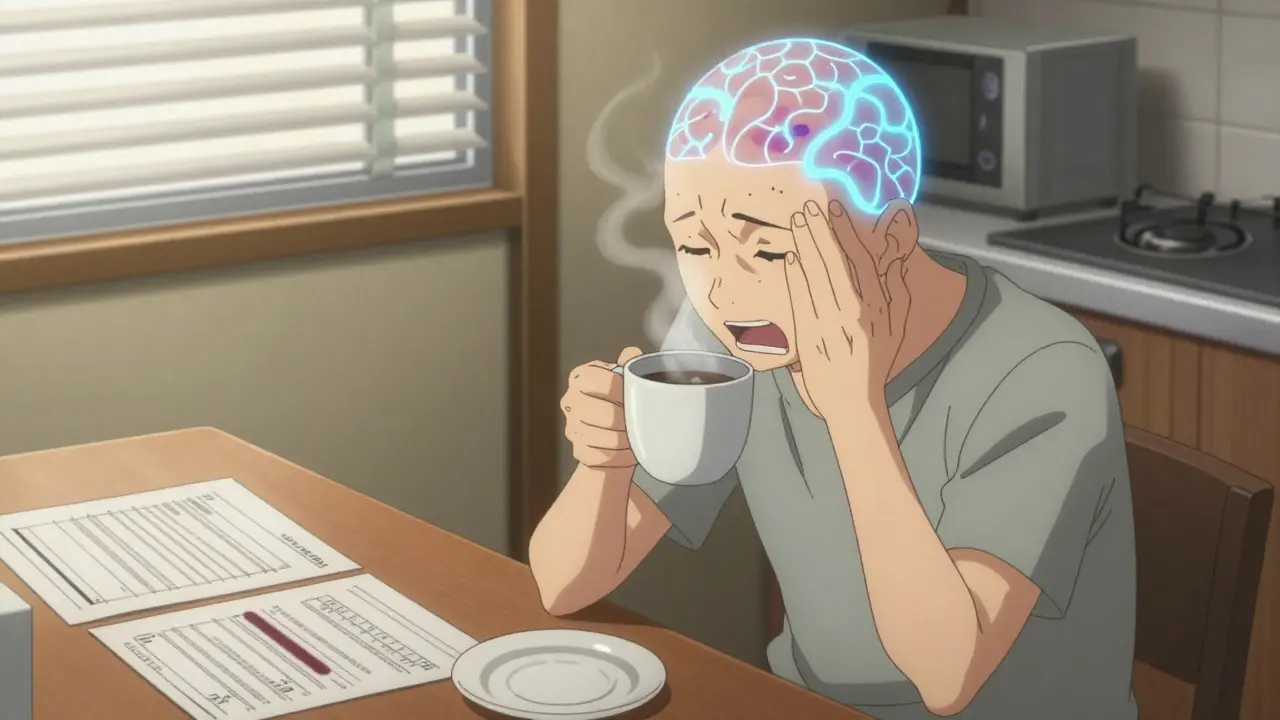
The most common sign? Tremor. About 7 out of 10 people who experience neurotoxicity from tacrolimus report uncontrollable shaking - usually in the hands, sometimes in the head or voice. It’s not just a little twitch. Patients describe it as being unable to hold a coffee cup, button a shirt, or sign their name. One transplant recipient on a patient forum said, ‘I dropped my spoon so many times I stopped eating in public.’
Headache is the second most frequent symptom. Not a normal tension headache. These are deep, constant, and often resistant to over-the-counter painkillers. People report them as ‘crushing,’ ‘pressure behind the eyes,’ or ‘like my skull is shrinking.’ One liver transplant patient on Reddit wrote: ‘I took 800 mg of ibuprofen every 6 hours for weeks. Nothing helped until they lowered my tacrolimus.’
Other symptoms pop up too: pins and needles in your fingers, trouble sleeping, dizziness, or feeling foggy. In rarer cases, people lose coordination, have trouble speaking, or even see double. These aren’t just side effects - they’re warning signs your brain is under stress.
Why It Happens - Even When Blood Levels Are ‘Normal’
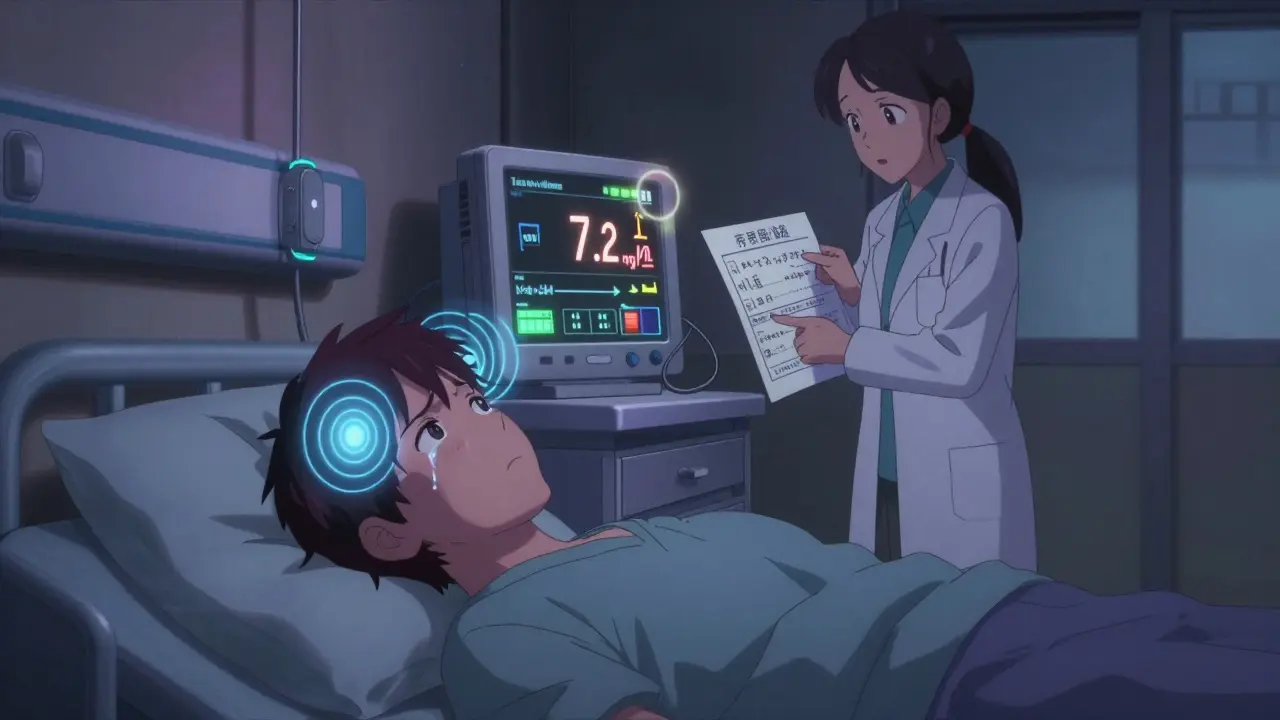
Doctors measure tacrolimus levels in your blood to make sure you’re in the safe range. For kidney transplants, that’s usually 5-15 ng/mL. For liver and heart, it’s 5-10 ng/mL. But here’s the problem: you can have a level of 7.2 ng/mL - perfectly within range - and still get severe tremors.
A 2023 study found that 21.5% of patients with early neurotoxicity had levels above 15 ng/mL. But here’s the twist: many patients with symptoms had levels that were technically normal. That means blood tests alone can’t predict who’s at risk.
Why? Because tacrolimus doesn’t just float in your bloodstream. It crosses into your brain. And not everyone’s brain lets it in the same way. Some people have a genetic variation called CYP3A5*1 that makes them absorb and process tacrolimus differently. These people are more likely to build up toxic levels in their brain, even if their blood test looks fine.
Also, other drugs can make things worse. Antibiotics like linezolid, sedatives like midazolam, or even antipsychotics like risperidone can team up with tacrolimus and push your brain over the edge. Electrolyte imbalances - especially low sodium - are another hidden trigger. One study showed correcting sodium levels alone helped 28% of mild cases without touching the tacrolimus dose.
Who’s Most at Risk?
Not all transplant patients are equally likely to get neurotoxicity. Liver recipients are hit hardest - around 36% report symptoms. Kidney recipients are next at 22%, then lung at 19%, and heart at 15%. Why? No one’s completely sure, but liver transplants often involve bigger doses, longer surgeries, and more complications that stress the body’s ability to handle the drug.
Age matters too. Older patients are more vulnerable. So are people with pre-existing nerve conditions, high blood pressure, or kidney problems. And if you’ve had neurotoxicity before, you’re far more likely to get it again.
There’s also a dangerous delay in diagnosis. A survey of transplant patients found that 55% waited 2-3 weeks before their medical team connected their symptoms to tacrolimus. That’s weeks of unnecessary suffering - and potential brain damage.
What to Do If You Have Symptoms
If you’re experiencing tremor, headache, or brain fog after a transplant, don’t wait. Don’t assume it’s ‘just stress’ or ‘normal recovery.’ Tell your transplant team immediately.
Here’s what usually happens next:
- Your tacrolimus level is checked - but don’t assume it’s the whole story.
- Your sodium, magnesium, and kidney function are tested.
- You’re asked about other medications you’re taking - even over-the-counter ones.
- If symptoms are moderate to severe, your doctor may lower your tacrolimus dose by 10-30%.
- If symptoms persist, they might switch you to cyclosporine, another immunosuppressant with lower neurotoxicity risk (though it has higher rejection risk).
Most patients see improvement within 3-7 days of a dose change. One patient on the National Kidney Foundation forum reported his tremor vanished in 72 hours after dropping his dose from 0.1 mg/kg to 0.07 mg/kg - even though his blood level stayed in range.
But here’s the catch: lowering tacrolimus increases your risk of rejection. That’s why this isn’t a decision you make alone. Your transplant team needs to balance the risk of your body attacking the organ against the risk of your brain shutting down.
What’s New in Managing This Problem
The field is changing. For years, doctors treated neurotoxicity like a side effect you just had to live with. Now, they’re starting to see it as a preventable issue.
In 2023, the American Society of Transplantation released its first-ever guidelines specifically for managing tacrolimus neurotoxicity. They now recommend routine neurological checks in the first 30 days after transplant - when symptoms are most likely to appear.
One of the most promising advances is genetic testing. If you know you carry the CYP3A5*1 gene, your doctor can start you on a lower dose from day one. A 2021 study showed this cut neurotoxicity risk by 27%. The problem? Most hospitals still don’t offer this test routinely because insurance won’t pay for it.
There’s also a new clinical trial called TACTIC, testing a smarter dosing algorithm that factors in your genetics, sodium levels, and blood pressure. Early results suggest it could reduce neurotoxicity by more than half.
And long-term? A new drug called LTV-1 is in early trials. It’s designed to work like tacrolimus but can’t cross the blood-brain barrier. If it works, it could be the first real alternative in decades.
What You Can Do Right Now
You don’t have to wait for new science to protect yourself. Here’s what you can do today:
- Track your symptoms in a notebook - when the tremor started, how bad the headache is, if you’re sleeping worse.
- Know your tacrolimus level - ask for a copy of your latest blood test.
- Review every medication you’re taking with your pharmacist - even aspirin or sleep aids.
- Ask if you’ve been tested for CYP3A5 genotype. If not, ask why.
- If you’re feeling off, speak up. Don’t wait for your next appointment.
Tacrolimus saved your life. But it shouldn’t steal your quality of life. You have the right to ask for better. You have the right to be heard. And you’re not alone - thousands of transplant patients are walking this same tightrope between survival and sanity.
Can tacrolimus cause tremors even if my blood level is normal?
Yes. Many patients develop tremors, headaches, or other neurological symptoms even when their tacrolimus blood levels are within the recommended therapeutic range (5-15 ng/mL). This is because individual differences in how the drug crosses the blood-brain barrier, genetic factors like CYP3A5 genotype, and interactions with other medications can cause brain-level toxicity without raising blood levels above normal. Studies show up to 30% of neurotoxicity cases occur at levels considered safe.
How long does it take for neurotoxicity symptoms to go away after lowering tacrolimus?
Most patients notice improvement within 3 to 7 days after reducing the tacrolimus dose or switching to another immunosuppressant. Tremor and headache often improve first, followed by sleep and cognitive clarity. In some cases, symptoms resolve completely within 72 hours. However, if symptoms are severe or linked to PRES or CIDP, recovery may take weeks or require additional treatments like IVIG or plasma exchange.
Is cyclosporine a safer alternative to tacrolimus for avoiding neurotoxicity?
Cyclosporine has a lower risk of neurotoxicity - about 15-20% lower than tacrolimus - which is why it’s often used as a switch option. However, it carries a higher risk of organ rejection (20-30% higher) and can cause more kidney damage and gum overgrowth. It’s not a perfect substitute, but for patients with severe neurotoxicity who don’t respond to dose adjustments, it can be a necessary trade-off. The decision should be made with your transplant team based on your rejection risk and overall health.
Can other medications make tacrolimus neurotoxicity worse?
Yes. Several common drugs can increase the risk or severity of neurotoxicity when taken with tacrolimus. These include antibiotics like linezolid, antifungals like fluconazole, sedatives like midazolam and propofol, and psychiatric medications like haloperidol, risperidone, and olanzapine. Even over-the-counter pain relievers like NSAIDs can affect kidney function and indirectly raise tacrolimus levels. Always review your full medication list with your pharmacist or transplant team before starting anything new.
Should I ask for genetic testing for CYP3A5 before starting tacrolimus?
It’s a smart question to ask. If you carry the CYP3A5*1 gene, you metabolize tacrolimus faster, which can lead to higher doses being prescribed - and higher brain exposure. Studies show that dosing based on CYP3A5 genotype reduces neurotoxicity by 27%. While most hospitals don’t offer this routinely due to cost and insurance barriers, it’s becoming more common in transplant centers. Ask if your center has a pharmacogenomics program or if testing is available through a research study.
Can low sodium levels trigger tacrolimus neurotoxicity?
Yes. Hyponatremia (low sodium levels below 135 mmol/L) is a known risk factor for tacrolimus neurotoxicity. It’s thought to make the blood-brain barrier more permeable, allowing more tacrolimus to enter the brain. In some cases, correcting sodium levels alone - without changing the tacrolimus dose - has been enough to resolve mild symptoms. This is why your doctor should check your electrolytes if you develop neurological symptoms.
Is PRES (Posterior Reversible Encephalopathy Syndrome) common with tacrolimus?
PRES is rare, occurring in only 1-3% of tacrolimus users, but it’s serious. It causes swelling in the back of the brain, leading to severe headaches, vision changes, seizures, or confusion. It shows up clearly on MRI scans as bright spots in the occipital lobes. If you develop sudden vision problems, seizures, or altered mental status, seek emergency care immediately. PRES usually reverses with prompt dose reduction or stopping tacrolimus, but delays can lead to permanent brain damage.

Comments
This post hit me right in the gut. I had tacrolimus tremors after my liver transplant - thought I was just anxious until my nurse noticed me spilling coffee all over my lap. Took three weeks for anyone to listen. Lowering my dose by 20% was like flipping a switch. My hands stopped shaking, and I finally slept through the night. You’re not crazy. You’re just medicated too hard.
They say it's 'normal' but they're just covering their asses. Pharma pushes tacrolimus because it's profitable. They don't care if you're shaking like a leaf or seeing double. The real fix? Get off the damn drug. But no - they'd rather you suffer quietly while they bill insurance for another 'follow-up.' They're not healers. They're salesmen with stethoscopes.
Low sodium can absolutely trigger this. Saw it in my unit - patient had tremors, headache, fog. Sodium was 132. Corrected it over 24 hours. Symptoms gone in 48. No dose change needed. Always check electrolytes first.
They’re hiding the truth. The real reason neurotoxicity is underreported? Because if patients knew how often this happens, they’d sue. They’d stop taking it. And then the organs would fail. So they call it ‘side effect’ and move on. The system doesn’t want you to know you have power. But you do. Ask for the genetic test. Demand it.
Thank you for writing this. I’m a kidney transplant mom and my son went through this. He didn’t say anything for weeks because he didn’t want to ‘be a burden.’ I found his notebook with scribbles: ‘Can’t hold spoon. Head feels like it’s being squeezed.’ We pushed for a dose change. He’s back to playing guitar now. You’re not alone. Speak up. We’ve got your back 💪❤️
Let me be clear - if your doctor tells you ‘it’s just stress’ or ‘you’re overthinking it’ when you have tremors, headaches, and brain fog post-transplant, that doctor is not doing their job. This isn’t anecdotal. This is documented, peer-reviewed, and preventable. The 2023 AST guidelines exist for a reason. Print them out. Bring them to your next appointment. If they don’t take you seriously, get a second opinion. Your brain matters more than their comfort zone. And yes, CYP3A5 testing should be standard. If your center doesn’t offer it, ask why they’re still practicing medicine in 2010.
My brother got switched to cyclosporine after his tremors got bad. He lost his kidney three months later. So yeah, cyclosporine might be ‘safer’ for your head - but your new organ doesn’t care. It just wants to survive. It’s a brutal trade-off. No one talks about how heavy that guilt is when you’re the reason your transplant failed. Don’t rush to swap drugs. Talk to your team. Weigh everything.
Wanted to add - if you’re on linezolid or fluconazole, stop taking them without telling your transplant team. Those two are silent killers when paired with tacrolimus. I’m a pharmacist. I’ve seen too many patients end up in ICU because someone just ‘grabbed’ an antibiotic from the pharmacy. Always run your med list by your transplant pharmacist. Seriously. They’re your secret weapon.