When a patient picks up a prescription and sees a pill that looks completely different from what they’ve been taking, it’s natural to wonder: Is this really the same medicine? Many patients assume the change means something’s wrong-maybe it’s weaker, less safe, or won’t work as well. But here’s the truth: it’s almost always the same drug. The difference isn’t in what heals them-it’s in what’s on the outside.
Why Generics Are Just as Effective
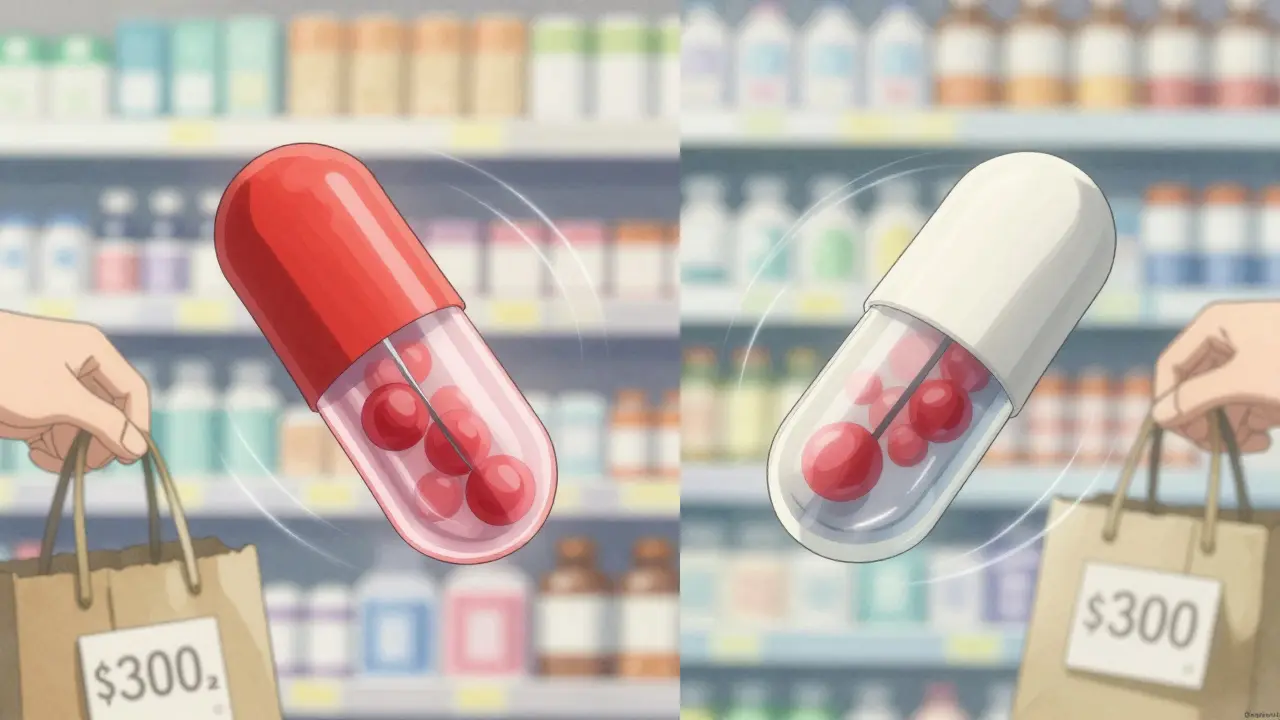
Generic medications aren’t knock-offs. They’re exact copies in every way that matters. The FDA requires them to contain the same active ingredient, in the same strength, taken the same way, and absorbed into the bloodstream at the same rate as the brand-name version. That’s not a suggestion-it’s a legal requirement. To get approved, a generic must prove it delivers between 80% and 125% of the brand’s drug levels in the body. That’s a tight range, and it’s backed by real testing in hundreds of volunteers.Think of it like two identical cars with different paint jobs. One’s a red Honda Civic, the other’s a white one. Same engine, same fuel efficiency, same safety features. The color doesn’t change how it drives. Generics work the same way. The active ingredient-the part that treats your condition-is identical. What changes are the fillers, dyes, and coatings. Those are inactive ingredients. They help the pill hold together or make it easier to swallow. But they don’t affect how the medicine works.
And the numbers don’t lie. In the U.S., 9 out of 10 prescriptions filled are for generics. Yet they make up less than a quarter of total drug spending. That’s because generics cost 80% to 85% less than brand-name drugs. For someone on a fixed income, that’s not just savings-it’s access. A Medicare patient switching from brand-name Crestor to generic rosuvastatin might save $300 a month. That’s rent money. That’s groceries. That’s keeping the medicine in their daily routine.
Why Patients Still Doubt Generics
Despite all the science, skepticism sticks. Why? Because patients aren’t reacting to data-they’re reacting to experience.When a patient gets a new pill that’s a different shape, color, or size, their brain flags it as unfamiliar. And if they’ve ever felt worse after a switch-maybe a headache, nausea, or just a sense that “it’s not working”-they blame the generic. But here’s the catch: most of those symptoms aren’t caused by the drug itself. They’re caused by the change. Switching medications-even to an identical one-can trigger side effects from the body adjusting. Or the patient might have been taking their old pill inconsistently and only noticed the difference when the pill changed.
Studies show that 28% of patients worry about switching from brand to generic. And 17% actually take their meds less often after the switch. That’s not because generics are inferior. It’s because they weren’t properly explained.
One Reddit thread from 2023 had over 140 pharmacist responses. The top concern? Appearance. 63% of patients refused generics because the pill looked different. Another 27% thought it wouldn’t work as well. Only 10% had a real negative experience. Yet, those fears are real to the person sitting in front of you.
The TELL Framework That Works
There’s no magic script. But there’s a proven structure: TELL.- Tell them it’s the same active ingredient. Say it plainly: “This generic has the exact same medicine in it as your old pill. It’s not a different drug-it’s the same one, just made by another company.”
- Explain why it looks different. “The color and shape are different because of trademark laws. The brand-name company owns how their pill looks. We can’t copy it, even if we wanted to. But the medicine inside? Identical.”
- Listen without interrupting. Don’t assume they’re being irrational. Ask: “What’s your biggest concern about this change?” Let them say it. Sometimes it’s cost. Sometimes it’s fear. Sometimes it’s a bad experience with a different generic last year. You can’t fix what you don’t understand.
- Link it to their goals. “I know you want to avoid hospital visits. This generic will do the same job as your brand, and save you over $200 a month. That money could go toward your co-pays, your groceries, or even your next doctor visit.”
One pharmacist in Birmingham told me about a patient on warfarin who refused generics after a previous switch. She didn’t push. She asked: “What happened the last time you switched?” The patient said, “I felt dizzy.” Turns out, he’d been traveling and missed doses. The dizziness wasn’t from the generic-it was from inconsistent use. Once she explained that, he agreed to try again-and stayed on it for two years.
What to Say When They Ask the Hard Questions
Patients will ask the same things over and over. Be ready.- “Is this really the same medicine?” → “Yes. Same active ingredient, same dose, same effect. The FDA requires this. If it weren’t the same, they wouldn’t approve it.”
- “Why does it look different?” → “The brand-name company owns the design. We can’t copy it. But the medicine inside? Same as always.”
- “Is it as strong?” → “It has to be. The FDA tests it to make sure it releases the same amount of medicine into your body. If it didn’t, it wouldn’t be sold here.”
- “I heard generics aren’t as good.” → “That’s a myth. A review of 47 studies with over 9,000 patients found no difference in effectiveness between generics and brands for heart disease, diabetes, or high blood pressure.”
Use the teach-back method. After explaining, ask: “Can you tell me in your own words why this generic is safe to take?” If they can, they’ve understood. If they can’t, you haven’t finished yet.
When Generics Aren’t the Answer
Not every drug is a simple swap. For medicines with a narrow therapeutic index-like levothyroxine for thyroid disease, warfarin for blood thinning, or certain seizure drugs-small changes in blood levels can matter. That’s why pharmacists are trained to watch these closely. But even here, switching between generics from the same manufacturer is safe. The risk comes from switching between multiple different manufacturers, which can cause slight variations in how the drug is absorbed.That’s why it’s important to stick with the same generic brand if possible. If a patient has been stable on one generic, don’t switch them to another unless necessary. And if they’ve had a bad experience before, ask: “Which one did you take last?” Then try to match it.
There’s also something called an “authorized generic”-a brand-name company’s own generic version. It’s made in the same factory, with the same formula. It looks almost identical. If a patient is really resistant, offering this as an option can ease the transition. It’s still cheaper than the brand, but feels more familiar.

What Happens When You Don’t Talk About It
Skipping the conversation isn’t neutral. It’s dangerous.Patients who aren’t counseled are 22% less likely to stick with their medication six months later. That means higher hospitalization rates, worse outcomes, and more cost to the system. It also means more frustration for you-the provider-who sees a patient come back because their condition isn’t controlled, and you know the answer was in their medicine cabinet all along.
One study found that when pharmacists spent just 3 to 5 minutes explaining generics, patient satisfaction jumped from 42% to 78%. That’s not luck. That’s communication.
What’s Changing Now
The FDA is investing $5 million in patient education for generics in 2026. They’re testing video explanations-short clips patients can watch on tablets in the pharmacy. Early results show these videos boost acceptance by 31% over talking alone. That’s because people remember stories and visuals better than facts.And it’s not just pills anymore. Biosimilars-complex generics for biologic drugs like insulin or rheumatoid arthritis treatments-are entering the market. These aren’t simple pills. They’re injectable therapies with more variables. The same communication principles apply, but the stakes are higher. Patients need to understand: “This isn’t a copy. It’s a scientifically proven match.”
For now, the message is simple: Generics save lives because they make treatment affordable. But they only work if patients take them. That’s why your words matter more than your prescription pad.
Are generic medications really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage, and route of administration as the brand-name version. They must also prove they deliver the same amount of medicine into the bloodstream at the same rate. Studies involving over 9,000 patients show no meaningful difference in effectiveness for conditions like high blood pressure, diabetes, or heart disease.
Why do generic pills look different from brand-name ones?
Trademark laws prevent generic manufacturers from copying the exact appearance of brand-name pills. That includes color, shape, and markings. But these differences are only cosmetic. The medicine inside is identical. The inactive ingredients-like dyes or fillers-may vary, but they don’t affect how the drug works.
Can switching to a generic cause side effects?
Switching itself can sometimes cause temporary side effects-not because the generic is inferior, but because the body is adjusting to a new pill, even if the medicine is the same. If a patient reports feeling worse after a switch, it’s important to check if they’re taking it consistently, or if they switched between multiple generic manufacturers. For drugs like levothyroxine or warfarin, sticking with the same generic brand is recommended.
Do generics cost less because they’re lower quality?
No. Generics cost less because they don’t need to repeat expensive clinical trials. The original brand paid millions to prove safety and effectiveness. Generics use that data and only test to prove they work the same way. They’re made in the same FDA-inspected facilities, under the same quality rules. The lower price is due to competition, not lower standards.
What should I do if a patient refuses a generic?
Don’t force it. Ask why they’re refusing. Is it the appearance? A past bad experience? Cost concerns? Use the TELL method: Tell them it’s the same medicine, Explain why it looks different, Listen to their concerns, and Link the savings to their personal goals. If they’re still unsure, ask if they’d be open to an authorized generic-made by the original brand but sold at generic prices.
Next Steps for Providers
Start small. Pick one patient this week who’s on a chronic medication and explain their generic option before they leave. Use the TELL method. Ask them to repeat it back. Write down their concerns in their file. You’ll be surprised how often they come back and say, “That generic worked fine.”The goal isn’t to convince everyone. It’s to give them the truth-clear, calm, and confident. Because when patients understand, they take their medicine. And when they take their medicine, they stay healthy.


Comments
Man, I love how this breaks it down. I’m a pharmacist in Ohio, and I’ve seen so many patients panic because their pill changed color. One lady cried because her blue pill turned white-she swore it ‘wasn’t the same medicine.’ I showed her the FDA label on the bottle, then pulled up the bioequivalence data on my tablet. She stared at it like it was magic. Then I said, ‘Your blood doesn’t care what color the pill is.’ She laughed. Took the script. Came back two weeks later with a thank-you note. That’s the stuff that keeps me in this job.
Generics aren’t just cheaper-they’re lifelines. I’ve had patients choose between insulin and rent. When they switch to generic, they don’t just save money-they survive. And yeah, sometimes they feel weird after a switch. But it’s rarely the drug. It’s the change. The brain hates surprises, even good ones.
Also, authorized generics? Total game-changer. I keep a few on hand just for stubborn patients. Same factory, same formula, just without the fancy branding. It’s like handing someone their favorite coffee in a plain cup. They’re like, ‘Wait, this tastes the same?’ Yep. And it costs half.
Teach-back is everything. Ask them to explain it back. If they can’t, you didn’t explain well enough. Not because they’re dumb. Because medicine is scary. And we’re the ones who make it feel safe.
Also, side note: I’ve had patients ask if generics are made in China and if they’re ‘safe.’ I say, ‘The FDA inspects every facility, no matter where it is. If it’s sold here, it passed the same tests as the brand.’ Then I ask, ‘Would you eat a banana from Mexico because it’s cheaper? Or refuse it because it’s not from California?’ They always laugh. Then they get it.
Bottom line: Your words matter more than your prescription pad. Always.
And if you’re a provider reading this-do this. Even if it takes 3 minutes. It changes lives.
India makes 60% of the world’s generic drugs and you people still doubt them? I mean really. We produce medicines for the entire Western world, and now you’re scared because your pill looks different? The FDA tests every batch. If you think Indian-made generics are inferior, you’ve never seen a GMP-certified facility in Hyderabad. The quality control is stricter than some American hospitals.
Also, your brand-name drugs? They’re often made in India too. Just with a different label. You’re paying for a logo. Not better medicine.
Stop being so dramatic. Your body doesn’t care if it’s blue or white. It cares if the molecule is there. And it is.
I've had patients refuse generics because they thought the color meant it was weaker. I just said 'if you can't tell the difference between a red car and a white one driving down the highway, you're probably not driving very well.' They laughed. Took the script. Never looked back. Simple truth: the pill doesn't care what it looks like. Your body does. And it works the same.
Thank you for this comprehensive breakdown. As a primary care provider, I’ve seen firsthand how misinformation around generics leads to non-adherence. The TELL framework is not just practical-it’s essential. I’ve started using it in every consult involving a switch, and my refill rates have improved by nearly 30%. The teach-back method, in particular, has been transformative. Patients who can articulate why the generic is safe are far more likely to stay on therapy.
Also, the data on biosimilars is encouraging. As these become more common, we’ll need to apply the same principles: clarity, empathy, and evidence. The science is solid. Our job is to make sure patients understand it.
Oh my god YES. I’m a diabetic and switched from brand-name insulin to generic last year. The pharmacy gave me this tiny, pale yellow vial. I almost threw it out. Felt like I was being scammed. Then my pharmacist sat me down and said, ‘This is the same stuff, just without the glitter.’ I asked what glitter meant. She said, ‘The brand spent millions on marketing, packaging, and that fancy blue box. This? Just the insulin.’
Turns out, I was having weird lows because I was skipping doses when I traveled. The switch didn’t cause it. My chaos did.
Now I tell everyone: if your pill looks like it was made in a cereal box, that’s a good thing. It means you’re not paying for a logo. You’re paying for science. And science doesn’t need a rainbow.
Also, authorized generics? They’re like your favorite hoodie from the same brand, but on sale. Same fabric. Same comfort. Just no tag. And you’re saving $200 a month. That’s a weekend trip. Or a new pair of shoes. Or not choosing between meds and food. I’m not crying. You’re crying.
Let me tell you something no one else will. I’ve worked in 12 pharmacies across three states. I’ve seen patients refuse generics because they thought the pill looked ‘cheap.’ One man told me, ‘If it’s not pink, it’s not working.’ I asked him if his iPhone was less powerful because it had a matte black case instead of white. He paused. Then he said, ‘…that’s a good point.’
But here’s the real issue: pharmacies switch manufacturers constantly. One month it’s Mylan, next month it’s Teva, then it’s Sandoz. And guess what? Some people *do* react differently between generics from different manufacturers. Especially with thyroid meds or warfarin. It’s not placebo. It’s bioavailability variance. The FDA allows up to 20% variation between brands. That’s not nothing.
So yes, generics are mostly fine. But don’t pretend switching between 5 different generics is the same as staying on one. That’s where the real risk is. And no one talks about it. Because it’s inconvenient.
Also, if your patient says ‘I feel weird,’ don’t dismiss it. Ask: ‘Which generic did you take before?’ Because sometimes, the answer is: ‘The one from the other pharmacy.’
And if you’re a provider who says ‘it’s all the same’-you’re not being helpful. You’re being lazy.
WHY ARE WE STILL TALKING ABOUT THIS?!
THE FDA DOESN’T APPROVE ‘KNOCK-OFFS’-IT APPROVES IDENTICAL DRUGS. PERIOD.
WHEN YOU SAY ‘IT LOOKS DIFFERENT’-YOU’RE SAYING ‘I TRUST THE BRAND NAME MORE THAN THE LAW.’
THEY’RE THE SAME DRUG. SAME MOLECULE. SAME DOSAGE. SAME BLOOD LEVELS. SAME CLINICAL OUTCOMES.
IF YOU’RE STILL DOUBTING IT-YOU’RE NOT DOUBTING THE MEDICINE.
YOU’RE DOUBTING YOURSELF.
AND THAT’S A PROBLEM.
THEY’RE NOT ‘CHEAPER.’ THEY’RE ‘EQUITABLE.’
AND IF YOU’RE TOO SCARED TO TAKE A WHITE PILLS BECAUSE YOUR OLD ONE WAS BLUE-
YOU NEED TO RECONSIDER EVERYTHING.
THEY’RE NOT ‘GENERIC.’ THEY’RE ‘STANDARD.’
AND WE’RE ALL STUPID FOR STILL HAVING THIS CONVERSATION IN 2025.
I swear, I took a generic for my blood pressure and it didn't work at all. I went back to the brand and boom, fine. So maybe they're not always the same?
Let’s be real-FDA bioequivalence standards are based on healthy volunteers, not people with comorbidities, renal impairment, or polypharmacy. The 80–125% range is a statistical loophole. What happens when you’re on 7 other meds? The pharmacokinetics get messy. The data doesn’t reflect real-world complexity. And let’s not forget: generics aren’t required to do long-term outcome studies. So yeah, maybe it works for 90% of people. But for the 10% who are metabolizing differently? They’re just… out of luck.
Also, manufacturing variability? It’s real. Different fillers = different dissolution rates. And if you’re on warfarin? That 5% difference could mean a clot or a bleed. We’re playing Russian roulette with pharmacogenomics.
And don’t get me started on biosimilars. These aren’t generics. They’re complex biologics. If you think they’re interchangeable without monitoring, you’re not a clinician-you’re a marketer.