Obesity Medication Dosing Calculator
This tool calculates correct weight metrics used in medication dosing for obese patients. Different drugs require different weight calculations to avoid underdosing or toxicity.
Input Your Measurements
Why This Matters
Example: For ceftriaxone (antibiotic), standard dosing by total body weight leads to treatment failure in 63% of obese patients. Adjusted body weight dosing can cut surgical site infections from 14.2% to 8.7%.
Remember: This tool provides weight metrics for dosing guidance, but therapeutic drug monitoring (TDM) is often the best way to ensure proper dosing, especially for critical medications.
When you’re obese, your body doesn’t just carry extra weight-it changes how medicines work. A 200-pound person doesn’t just need a bigger pill than a 150-pound person. The way drugs move through the body, where they go, how fast they’re broken down, and how long they last-all of it shifts with body fat. This isn’t theory. It’s happening in hospitals every day, and it’s causing real harm when ignored.
Why Standard Doses Fail in Obese Patients
Most drug labels still list dosing based on average body weight. But in someone with obesity, that standard dose often doesn’t work. Why? Because fat tissue changes how drugs behave. Some medicines dissolve easily in fat, others don’t. Some are cleared quickly by the liver or kidneys, and in obesity, those organs work differently.
Take antibiotics like ceftriaxone. A typical dose is 1 gram once a day. But in a patient with a BMI over 30, that dose drops below effective levels in 63% of cases. The drug doesn’t reach the infection site in enough concentration. The result? Treatment fails. Infections come back. Surgeries get infected. At UCSF, switching to a minimum 2-gram dose for obese patients cut surgical site infections from 14.2% to 8.7%.
On the flip side, some drugs build up too much. Voriconazole, used for serious fungal infections, reaches toxic levels in 39% of obese patients when dosed by total body weight. That can cause liver damage, hallucinations, or vision problems. But when doctors use adjusted body weight instead, those dangerous spikes drop to just 12%.
Understanding Body Weight Metrics: TBW, IBW, AdjBW, LBW
Doctors don’t just guess. They use formulas to estimate what part of your weight actually matters for dosing.
- Total Body Weight (TBW): Your actual weight on the scale. Often wrong for dosing.
- Ideal Body Weight (IBW): The weight you’d have if you had normal body fat. For men: 50 kg + 2.3 kg for every inch over 5 feet. For women: 45.5 kg + 2.3 kg per inch over 5 feet.
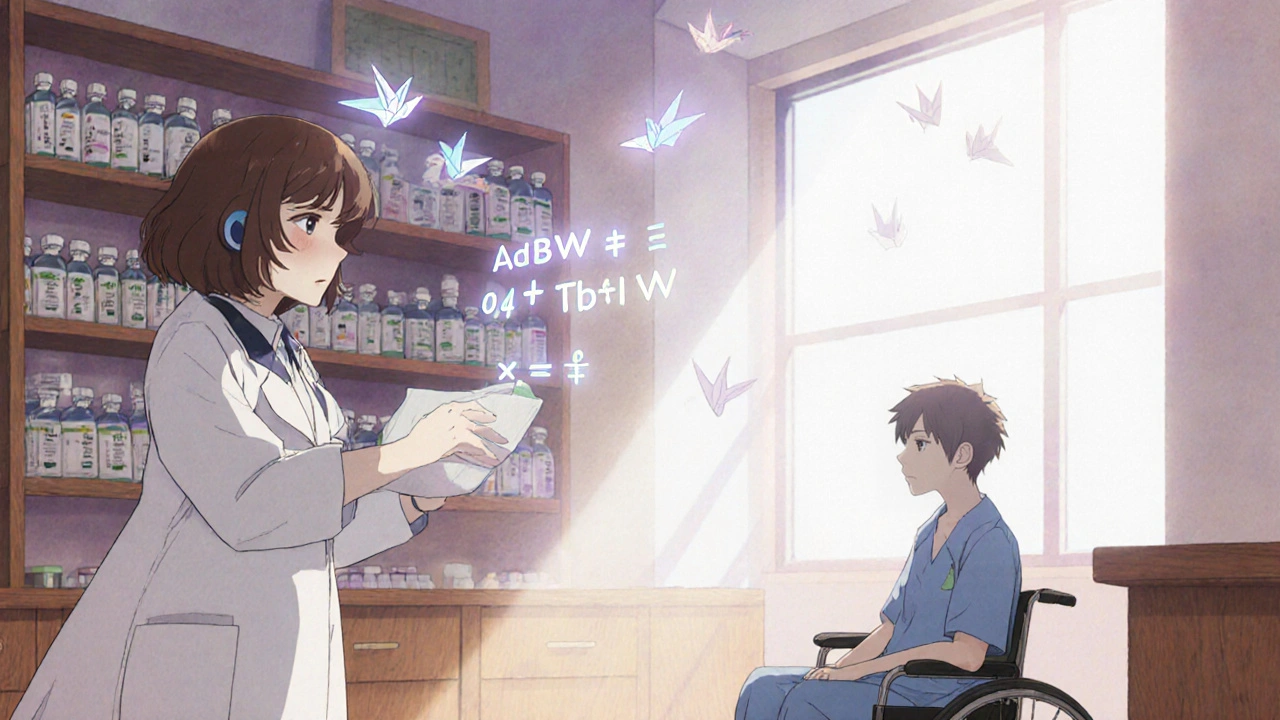
- Adjusted Body Weight (AdjBW): A middle ground. Formula: IBW + 0.4 × (TBW − IBW). Used for many antibiotics like ceftriaxone and vancomycin.
- Lean Body Weight (LBW): Your weight minus fat. Used for drugs that stick to fat, like diazepam or fentanyl.
For example, a woman who weighs 110 kg (242 lbs) and is 5’5” has an IBW of about 62 kg. Her AdjBW is 62 + 0.4 × (110 − 62) = 81.2 kg. That’s the number doctors use to calculate her antibiotic dose-not her full 110 kg.
How Different Drugs React to Obesity
Not all drugs act the same. Here’s what the data shows:
| Drug | Standard Dose | Obese Patient Dose | Why It Changes |
|---|---|---|---|
| Ceftriaxone (antibiotic) | 1 g daily | 2 g daily minimum | Increased clearance; hydrophilic |
| Voriconazole (antifungal) | Based on TBW | Based on AdjBW | Too much accumulates in fat; risk of toxicity |
| Enoxaparin (blood thinner) | 40 mg once daily | 40 mg twice daily (BMI 40-49.9) 60 mg twice daily (BMI ≥50) |
Higher volume of distribution; risk of clots if underdosed |
| Apixaban (blood thinner) | 5 mg twice daily | Same dose up to 85 kg, then 2.5 mg twice daily | Dichotomized dosing causes dangerous spikes in exposure above 85 kg |
| Tigecycline (antibiotic) | 100 mg load, 50 mg every 12h | 200 mg load, 100 mg every 12h (for resistant infections) | Increased volume and clearance; higher doses needed |
| Colistin (antibiotic) | Based on TBW | Max 360 mg colistin base activity (CBA) based on IBW | High risk of kidney damage in obese patients |
Notice the pattern? Hydrophilic drugs (like most antibiotics) need higher doses because they don’t mix with fat-they spread through water-rich tissues, which increase with obesity. Lipophilic drugs (like painkillers or sedatives) spread into fat, so their volume of distribution grows. Giving them standard doses leads to long, unpredictable effects.
Therapeutic Drug Monitoring: The Missing Safety Net
Formula-based dosing helps-but it’s not perfect. That’s why therapeutic drug monitoring (TDM) is becoming essential.
TDM means taking a blood sample to measure exactly how much drug is in your system. It’s routine for drugs like vancomycin and aminoglycosides in obese patients. At Stanford Health Care, using TDM for voriconazole cut toxic levels from 39% down to 12%. It also reduced the number of dose changes by over half.
The problem? Only 37% of U.S. hospitals have formal obesity dosing protocols. And even fewer have TDM programs. Pharmacists report that 63% of them want to use TDM but can’t because their hospital doesn’t support it.
For patients, this means you might be getting a dose that’s too low-or too high-and no one knows until something goes wrong.
What Happens When Dosing Is Wrong
Underdosing leads to treatment failure. A patient with a staph infection gets a standard antibiotic dose. The drug never reaches the infection. The wound doesn’t heal. The infection spreads. The patient is readmitted. The cost? Thousands more in hospital bills.
Overdosing leads to toxicity. A patient on high-dose enoxaparin gets a bleed. Someone on voriconazole loses their vision temporarily. A patient on apixaban has a stroke because their dose jumped too high after crossing the 85 kg threshold.
One study at the University of Michigan found 28% of medication errors in obese patients were due to confusion over which weight to use. One case involved a patient with BMI 52 who got double the right dose of heparin-leading to a life-threatening blood disorder.
These aren’t rare mistakes. They’re systemic failures.
Why Hospitals Are Slow to Change
Changing how drugs are dosed sounds simple. But it’s not.
Pharmacists need training. Electronic health records don’t auto-calculate AdjBW. Doctors don’t know the formulas. Nurses aren’t taught to question a standard dose for a heavy patient. And drug labels? Only 18% of FDA-approved drug labels include any obesity dosing guidance.
At Stanford, it took 8 weeks of training for staff to get comfortable with the new voriconazole protocol. At UCSF, switching to higher ceftriaxone doses caused temporary drug shortages because pharmacies weren’t stocked for 2-gram vials.
Even the tools are fragmented. Lexidrug, MediCalc, and DoseMe offer calculators-but not all hospitals use them. And if your hospital doesn’t have a protocol, you’re stuck guessing.
What You Can Do
If you’re obese and taking any medication-especially antibiotics, blood thinners, or antifungals-ask these questions:
- Is this dose based on my total weight, or my adjusted or ideal weight?
- Have you checked if I need a higher or lower dose because of my weight?
- Could therapeutic drug monitoring help me?
- Is there a published guideline for this drug in obese patients?
Don’t assume your doctor knows. Many don’t. Bring the information. Print out a reference from the Clincalc Obesity Dosing Table (updated weekly since 2018). It lists 147 drugs with evidence grades.
And if you’re on a blood thinner like apixaban, know this: the 85 kg cutoff isn’t arbitrary. It’s based on real data showing bleeding risk jumps at that point. If you’re just above it, your dose may need to drop-not rise.
The Future Is Personalized
Change is coming. The FDA now requires drug companies to test medications in obese patients. In 2024, they expanded that to include people with BMI over 50. The NIH just funded a $4.7 million study to track how drugs behave in obese patients over five years.
Soon, dosing won’t just be based on weight. It’ll be based on body composition-how much muscle, how much fat, how your liver processes drugs, even your genes. One expert predicts that within five years, we’ll use imaging scans and genetic tests to tailor every dose to the individual.
But until then, the gap remains. And the people most at risk are those who need better care the most.

Comments
Let me tell you about the time I saw a 300lb guy get 1g ceftriaxone for a septic wound. He coded 48 hours later. No one checked his BMI. The chart just said 'standard dose'. This isn't theory. It's murder by protocol.
Apixaban dose drops at 85kg? That's wild. My uncle took 5mg twice and bled out. They said 'obese = higher dose' but the data says the opposite.
As a pharmacist in rural Ohio, I've seen this firsthand. We don't have TDM. We don't have AdjBW calculators in the EHR. Nurses just wing it. I had to manually override a vancomycin dose for a 140kg patient last week. The system auto-filled 1g. I called the MD. He said 'he's fat, give him more'. I said 'no, he'll crash his kidneys'. We argued for 20 minutes. This system is broken.
My dad's on enoxaparin. He's 220 lbs. The script said 40mg once. I printed the Clincalc table and showed his doctor. They changed it to 40mg twice. He stopped getting clots. If I hadn't pushed, he'd be dead. Doctors don't know this stuff. You have to be your own advocate.
They're hiding the truth. Big Pharma doesn't want you to know that fat people need different doses. It's cheaper to keep giving the same pills. That's why only 18% of labels have obesity info. They'd rather kill you slowly than spend money on real studies. TDM? That's too expensive. Let the obese die quietly.
Oh please. This is just another 'fat people are broken' narrative. Why not fix the damn drugs instead of blaming the patient's body? Also, AdjBW is a pseudoscientific scam. BMI is a racist colonial tool. This whole post is just medical gaslighting wrapped in graphs.
bro i got a 2g dose of ceftriaxone once and my pee turned purple. now i think all doctors are just guessing. also why do they even use kg? we live in america. use pounds. and why do i need to know what adjbw is? just give me the right dose. thanks.
Is there any data on how body fat distribution (visceral vs subcutaneous) affects drug distribution? Or is everything still just based on BMI and weight?
Correction: The study at the University of Michigan found 28% of medication errors in obese patients were due to confusion over which weight metric to use-not 'confusion over weight' as implied. Precision matters. Also, the FDA’s 2024 requirement applies to new drugs, not existing ones. Please cite accurately.
As a clinical educator with over 25 years in hospital pharmacy, I have witnessed the evolution of obesity-related dosing from near-total neglect to incremental progress. The challenges are multifaceted: institutional inertia, lack of standardized electronic health record integration, and a persistent cultural bias that equates higher body weight with noncompliance or lack of self-care. The solution lies not in individual patient advocacy alone, but in systemic reform-mandatory pharmacotherapy training for all clinicians, integration of AdjBW calculators into EHRs, and reimbursement structures that incentivize therapeutic drug monitoring. Until we treat obesity as a physiological variable-not a moral failing-we will continue to harm the very patients we aim to help.
They're not just underdosing. They're erasing us. I had a friend die from a pulmonary embolism because they gave her 40mg enoxaparin. She weighed 280. They said 'it's standard'. She was 32. Now I don't trust any doctor. I don't trust any pill. I don't trust any hospital. This isn't medicine. It's eugenics with a stethoscope.
My sister's a nurse in Chicago. She told me they just started using AdjBW for vancomycin last month. Took 6 months of lobbying. But now, no one's getting toxic levels anymore. Small wins matter. Keep pushing. You're not alone.