What Happens When AKI Hits Chronic Kidney Disease?
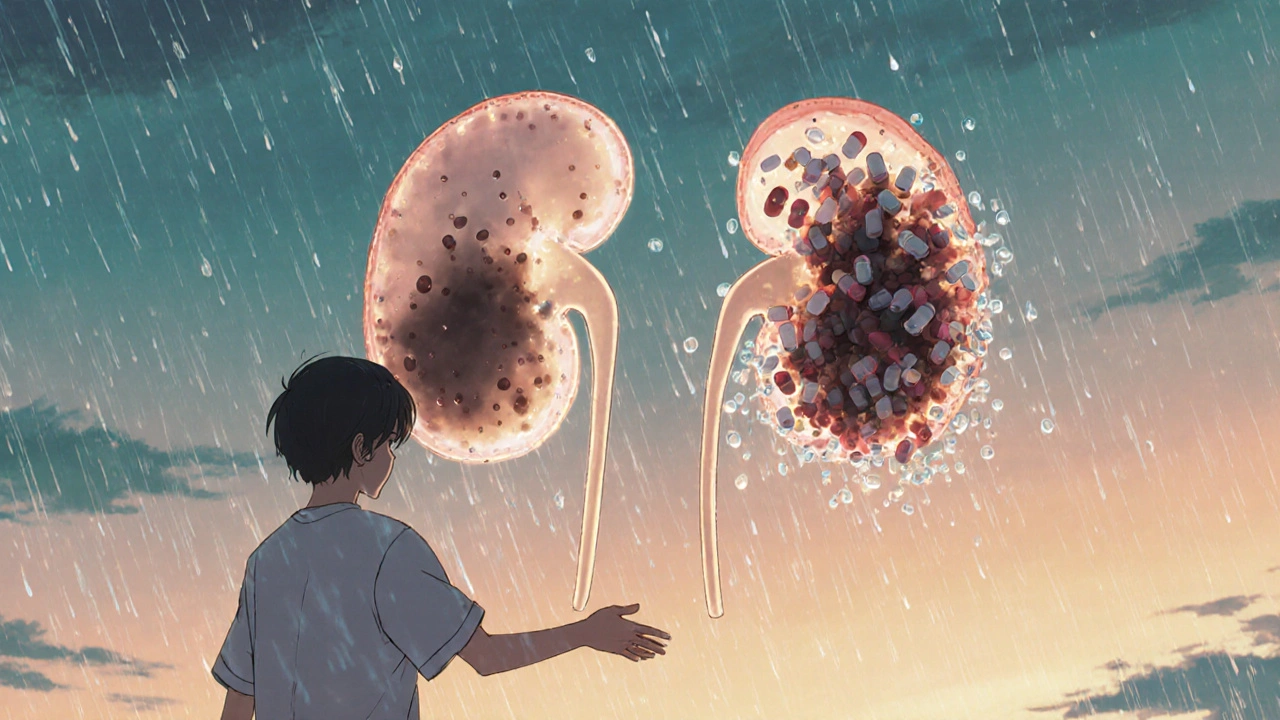
If you have chronic kidney disease (CKD), your kidneys are already working harder than they should. When an acute injury-called acute kidney injury, or AKI-happens on top of that, things can go south fast. This isn’t just a temporary bump. It’s a dangerous combo that can push you toward dialysis, hospitalization, or even death. The good news? You can prevent most of these episodes by avoiding two big triggers: contrast dye and nephrotoxic medications.
Think of your kidneys like a filter. In CKD, the filter is clogged. Contrast dye and certain drugs act like glue-they make the clog worse. And once that happens, recovery isn’t guaranteed. About 30% of AKI cases in people with CKD lead to permanent damage. Ten to fifteen percent end up needing long-term dialysis within five years. That’s not a small risk. It’s a warning sign you can’t ignore.
What Exactly Is AKI on CKD?
AKI means your kidneys suddenly lose function-within hours or days. CKD means they’ve been struggling for months or years. When AKI happens on top of CKD, your kidneys don’t have the reserve to bounce back. This isn’t just a lab value change. It’s a life-threatening event.
The KDIGO guidelines (used worldwide) define AKI by three things: a rise in creatinine by 0.3 mg/dL or more within 48 hours, a 50% jump from your baseline, or urine output dropping below 0.5 mL per kg per hour for more than six hours. For someone with CKD, even a small creatinine spike can mean serious trouble. Your baseline is already low. A 50% rise might take you from 2.0 to 3.0-and that’s not just a number. It’s a red flag.
Doctors now recognize that if kidney damage lasts more than seven days, it’s not just AKI-it’s acute kidney disease (AKD). That means your kidneys aren’t recovering like they should. You need follow-up tests at three months to see if it’s turned into worse CKD.
Why Contrast Dye Is So Dangerous
Contrast dye is used in CT scans, angiograms, and other imaging tests to make blood vessels and organs show up clearer. But for people with CKD, especially those with eGFR under 60, it’s a gamble.
Studies show that 12% to 50% of CKD patients develop contrast-induced AKI after receiving iodinated contrast. That risk jumps to 20-50% if you also have diabetes or heart failure. And if you’re dehydrated? The risk shoots up again.
Here’s what the guidelines say: avoid contrast if you can. If you absolutely need it-like for a life-threatening emergency-use the smallest dose possible (usually under 100 mL). Hydrate with normal saline before and after. The standard is 1.0 to 1.5 mL per kg per hour for 6 to 12 hours before and after the scan. That’s about 2 to 3 liters for most adults. Don’t rely on water alone. Saline works better.
Some hospitals now use cystatin C instead of creatinine to check kidney function before scans. Why? Creatinine can be misleading. If you’ve lost muscle mass (common in older adults or those with CKD), your creatinine might look normal even when your kidneys are failing. Cystatin C doesn’t depend on muscle, so it’s more accurate.
And no-N-acetylcysteine (NAC) isn’t a magic shield. Some studies say it helps. Others say it doesn’t. The evidence is mixed. Hydration is still your best bet.
Nephrotoxic Medications: The Silent Killers
Contrast dye gets all the attention. But the real daily threat? The pills and IVs you’re already taking.
NSAIDs-like ibuprofen, naproxen, and celecoxib-are the biggest offenders. They block prostaglandins, which help your kidneys stay healthy when blood flow is low. In CKD, that’s a disaster. The Veterans Health Administration found NSAID use increases AKI risk by 2.5 times in CKD patients. That’s not a typo. It’s a 150% jump in danger.
And you might not even realize you’re taking them. Many people pop Advil for headaches or back pain. Others take prescription NSAIDs for arthritis. If you have CKD, you need to stop them cold. Acetaminophen (Tylenol) is safer-but don’t overdo it. More than 3,000 mg a day can hurt your liver, and that’s another problem.
Then there are antibiotics. Aminoglycosides (like gentamicin) damage kidneys in 10-25% of courses. Vancomycin? Nephrotoxic in 5-40% of cases, especially if blood levels go above 15 mcg/mL. Amphotericin B? Up to 80% of patients on it get kidney damage. These aren’t rare. They’re common in hospitals.
Even blood pressure meds can be risky. ACE inhibitors and ARBs are great for CKD-they protect your kidneys long-term. But during AKI, they can cause a sudden spike in creatinine. That doesn’t mean you should quit them. It means you need to adjust. Abruptly stopping them can cause a 15-25% creatinine rise. Talk to your doctor. Don’t stop on your own.
What Medications to Avoid (and What to Use Instead)
Here’s a simple list of what to skip and what’s safer:
- Avoid: NSAIDs (ibuprofen, naproxen, diclofenac), aminoglycosides (gentamicin, tobramycin), vancomycin (unless closely monitored), amphotericin B, contrast dye (unless essential), diuretics (unless you’re fluid overloaded), dopamine (never for kidney protection)
- Safer alternatives: Acetaminophen for pain, penicillins or cephalosporins for infections (if kidney-safe doses), hydration with saline, non-contrast imaging (ultrasound, MRI without contrast)
Pharmacists are your secret weapon. A 2023 study showed pharmacist-led reviews cut AKI rates in CKD patients by 22%. They check your meds, flag interactions, and tell your doctor when something’s risky. Ask for a med review if you’re hospitalized or starting new drugs.
Hydration, Monitoring, and the Right Care Team
Hydration isn’t just drinking water. It’s getting the right fluid, at the right time, in the right amount. Normal saline is the gold standard. Avoid dextrose, albumin, or hydroxyethyl starch-they don’t help and can make things worse.
Monitor your creatinine closely. In stable CKD, you check it every 3-6 months. During AKI, check it every 24-48 hours. If you’re in the hospital, make sure someone is tracking it daily. Don’t assume they are. Ask.
And don’t wait for symptoms. AKI often has no pain, no swelling, no warning. You might just feel tired. That’s it. That’s enough reason to get tested.
When things get serious, nephrologists save lives. A 2020 study found that patients with AKI on CKD who saw a kidney specialist had 20% lower mortality. If you’re hospitalized with rising creatinine, ask: “Can I get a nephrology consult?”
What You Can Do Right Now
You don’t need to wait for a crisis. Here’s your action plan:
- Know your eGFR. If it’s below 60, you have CKD. If it’s below 30, you’re in high-risk territory.
- Make a list of every medication you take-prescription, over-the-counter, supplements. Bring it to every appointment.
- Ask your doctor: “Is this test or drug safe for my kidneys?” Always.
- Stop NSAIDs. Use acetaminophen instead. If you need stronger pain relief, talk to your doctor about alternatives.
- Hydrate daily. Drink enough water so your urine is light yellow. Avoid dehydration, especially if you’re sick, sweating, or in hot weather.
- Get a pharmacist to review your meds. Many pharmacies offer free med reviews.
- If you’re scheduled for a CT scan, ask: “Can we do it without contrast? If not, can I get saline before and after?”
Studies show that CKD patients who get clear advice on avoiding NSAIDs and staying hydrated have 25% fewer AKI hospitalizations. Knowledge isn’t power-it’s protection.

What’s New in 2025?
The KDIGO guidelines are being updated in late 2024. New evidence shows that sodium bicarbonate hydration doesn’t help more than normal saline. Also, early dialysis doesn’t improve outcomes in severe AKI. So, don’t rush to dialysis unless you’re in true crisis.
Biomarkers like TIMP-2 and IGFBP7 are now being used in ICUs to predict AKI 12 hours before creatinine rises. These tests aren’t common yet, but they’re coming. If you’re in the hospital and they test for them, it’s a good sign-they’re taking your kidney risk seriously.
Electronic alerts in hospital systems flag nephrotoxic drugs for CKD patients. But here’s the catch: 40% of doctors override them because they think the patient “needs it.” That’s why you have to be your own advocate. If you see an alert on your chart, ask why the drug is still being given.
Final Thought: Your Kidneys Can’t Speak. You Have To.
AKI on CKD isn’t something that just happens. It’s usually preventable. Most cases happen because someone didn’t ask the right questions. Maybe the doctor didn’t know your eGFR. Maybe you didn’t tell them you took ibuprofen for your back. Maybe the nurse didn’t hydrate you before the scan.
You hold the power here. Know your numbers. Speak up. Say no to NSAIDs. Ask about contrast. Get your meds reviewed. Hydrate. That’s not just advice-it’s your lifeline.
Can I still get a CT scan if I have CKD?
Yes, but only if absolutely necessary. Always ask if a non-contrast scan (like ultrasound or MRI without dye) will work. If contrast is required, make sure you’re hydrated with normal saline before and after. The dose should be kept under 100 mL. Tell the radiology team your eGFR and that you have CKD. They have protocols for high-risk patients.
Is Tylenol safe for CKD patients?
Yes, acetaminophen (Tylenol) is the safest pain reliever for CKD patients. But don’t exceed 3,000 mg per day. Higher doses can damage your liver, especially if you drink alcohol or have fatty liver disease. Always check with your doctor if you’re taking other medications that also contain acetaminophen, like cold or sleep aids.
Why can’t I take ibuprofen if I have CKD?
NSAIDs like ibuprofen block chemicals your kidneys need to maintain blood flow, especially when you’re dehydrated or have reduced kidney function. In CKD, your kidneys are already struggling. Taking NSAIDs can cause a sudden drop in kidney function-sometimes within days. Studies show it increases AKI risk by 2.5 times. It’s not worth the risk.
Should I stop my ACE inhibitor or ARB if I get AKI?
No-don’t stop them on your own. These drugs protect your kidneys long-term. A temporary rise in creatinine (15-25%) after starting or increasing them is normal and doesn’t mean they’re hurting you. But if your creatinine rises more than 30% or you develop high potassium or low blood pressure, your doctor may need to adjust the dose. Never stop without medical advice.
How often should I get my kidney function checked?
If you have stable CKD, check your eGFR and urine albumin-to-creatinine ratio (uACR) every 6-12 months. If you’ve had AKI, get checked every 2-4 weeks after the event, then every 3 months for a year. If your kidney function doesn’t return to baseline after 3 months, you may have developed chronic kidney disease (CKD) or acute kidney disease (AKD). Follow-up is critical.
Can drinking more water prevent AKI?
Yes-but not just any water. For AKI prevention, especially before contrast, isotonic saline (normal saline) is proven to help. Drinking plain water helps with general hydration, but it doesn’t replace the need for IV fluids in high-risk situations. If you’re at risk, aim for 2-3 liters of fluids daily, and more if you’re sweating, sick, or getting a scan. Avoid alcohol and caffeine, which can dehydrate you.
Do I need to see a nephrologist if I have CKD?
Not every CKD patient needs a nephrologist, but you should if your eGFR is below 30, if you have protein in your urine, if you’ve had AKI, or if your kidney function is worsening. Studies show that patients who see a kidney specialist have 20% lower death rates. Ask your doctor for a referral if you’re unsure.
Next Steps: Protect Your Kidneys Today
Don’t wait for a hospital stay to learn this. Start now:
- Get your eGFR and uACR tested if you haven’t in the last year.
- Make a list of every medication you take-including vitamins and herbal supplements.
- Remove all NSAIDs from your medicine cabinet. Replace them with acetaminophen.
- Ask your pharmacist to review your meds. Most offer this for free.
- If you’re due for a scan, call ahead. Ask: “What’s the plan to protect my kidneys?”
- Drink water daily. Don’t wait until you’re thirsty.
These aren’t just tips. They’re survival steps. Your kidneys can’t tell you when they’re failing. You have to speak for them. And when you do, you’re not just avoiding a bad lab result-you’re protecting your future.

Comments
This is so important... I had no idea NSAIDs were this dangerous for CKD. I've been taking ibuprofen for my back for years... 😳 I just called my doctor and switched to Tylenol. Hydration before scans? Done. Thank you for this. 🙏
The KDIGO guidelines are frankly underutilized in primary care. Most GPs don't even know what cystatin C is let alone when to use it. Contrast induced AKI is preventable but hospitals treat it like an inevitability. This post should be mandatory reading for med students.
I cannot believe how casually some clinicians dismiss nephrotoxicity. I am a nurse, and I have seen patients on vancomycin with no monitoring, NSAIDs prescribed without a second thought, and contrast administered without hydration protocols. This is not medical care-it is negligence dressed in white coats. Someone needs to be held accountable.
Let's be precise: the 12-50% contrast-induced AKI statistic is misleading without context. It's highly dependent on baseline eGFR, volume status, and comorbidities. The real issue is that many hospitals still use creatinine alone as a renal biomarker-despite its well-documented limitations in elderly and cachectic populations. Until we standardize cystatin C and point-of-care biomarkers, we're flying blind.
You guys are doing amazing work here 🙌 Seriously. I'm a CKD patient (eGFR 28) and this post literally saved me. I was about to get a CT with contrast last week until I read this and asked for an ultrasound instead. My doc was surprised I knew to ask. Now I'm getting my meds reviewed next week. You're not just giving info-you're giving people their lives back. ❤️
In the United States, we have a systemic failure in patient education. This information should be distributed in every primary care waiting room, pharmacy pamphlet, and Medicare guide. Knowledge is not optional when it comes to kidney health. It is the difference between independence and dialysis.
LMAO so now we gotta avoid all meds and just drink water? Cool. So my buddy with CKD just takes a nap when he feels tired and calls it a day? Yeah right. This post is like a 10 page essay on how to not die from breathing. Chill. Most people are just trying to live.
I almost died last year because my doctor didn't check my creatinine before a CT. I was in the ER for 5 days. My kidneys were at 18%. Now I have a list taped to my fridge. No NSAIDs. No contrast. No excuses. This isn't a suggestion. It's a survival manual.
Oh wow, another 'you must hydrate' post. Did you also consider that maybe your kidneys are just broken and no amount of water will fix it? Also, why are we blaming doctors? Maybe patients should stop popping ibuprofen like candy. And why do we assume everyone has access to a pharmacist? Not everyone lives in a CVS parking lot.
Okay but what if I just want to take Advil for my headache? Is my life not worth a little kidney stress? Also, I heard a guy on YouTube say dialysis isn't that bad. He's been on it for 10 years and says he's 'living his best life.' So maybe this whole 'avoid contrast' thing is just fearmongering?
This is why America is falling apart. We're too soft to take a little risk. Back in my day, we took NSAIDs, got contrast scans, and didn't cry about it. You think your kidneys are special? They're not. Stop being a hypochondriac and live your life.
To the person who said 'just live your life'... I'm not a hypochondriac. I'm the guy who almost didn't wake up after his creatinine hit 5.2. I'm the one who had to explain to my 8-year-old why he can't go to school because his dad was on dialysis for a week. You don't get to say 'just live' when you haven't lived this. I'm not risking it again. Not for a headache.