Lithium-NSAID Risk Assessment Tool
Understand Your Risk
This tool calculates your risk level based on key factors from the article. Your doctor should always confirm these results.
High Risk
Critical Action Required
Stop NSAID immediately. Contact your doctor within 24 hours. Monitor for symptoms of lithium toxicity: nausea, confusion, tremors, dizziness.
Get your lithium level checked within 72 hours. Avoid NSAIDs for at least 10 days.
When you're managing bipolar disorder with lithium, you're already walking a tightrope. Your doctor checks your blood levels regularly. You know to avoid dehydration. You watch for tremors or nausea. But there’s one hidden danger that even many doctors overlook: NSAIDs. That ibuprofen you grab for a headache, the naproxen for your arthritis, even the aspirin you thought was harmless-these can push your lithium levels into toxic territory, sometimes within days.
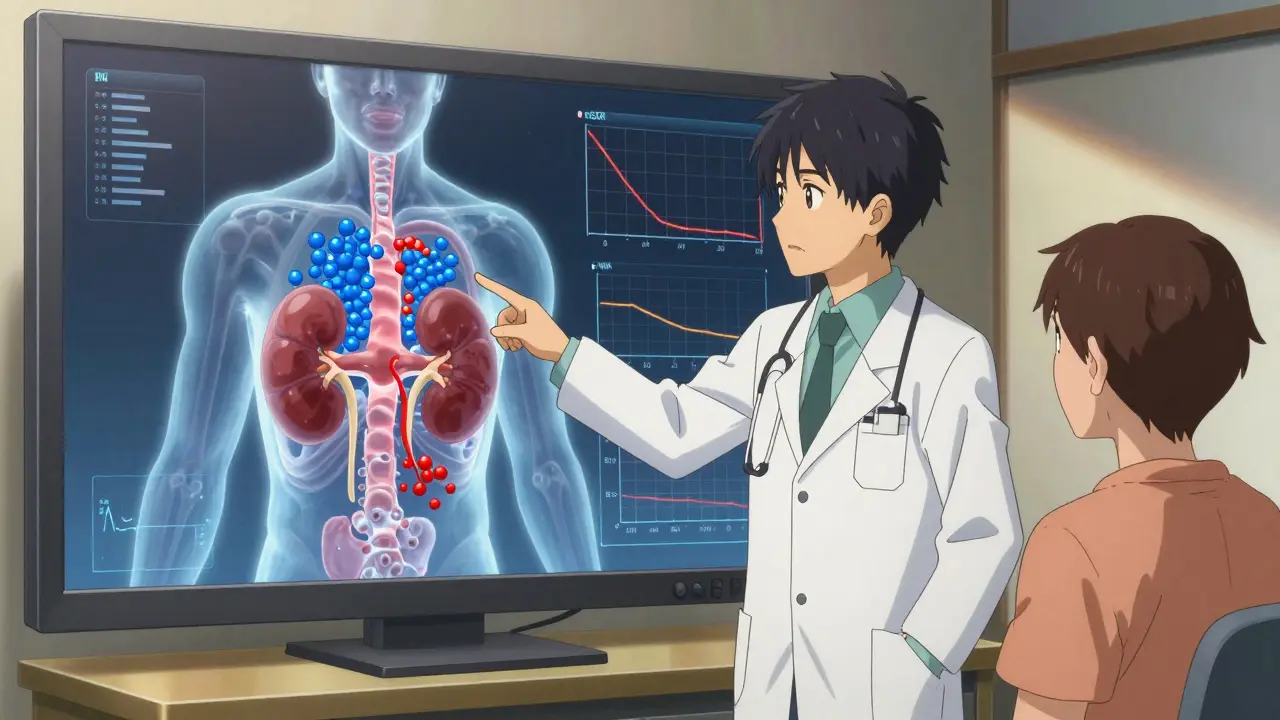
How NSAIDs Turn Lithium Into a Poison
Lithium works by stabilizing mood, but it’s a narrow therapeutic drug. The difference between a helpful dose and a dangerous one is small. Your kidneys handle lithium the same way they handle salt: they filter it out, but only if they’re working right. NSAIDs mess with that process. They block enzymes called COX-1 and COX-2, which your kidneys use to make prostaglandins. These prostaglandins help keep blood flowing to your kidneys. When NSAIDs shut them down, your kidneys slow down filtration. Lithium doesn’t get flushed out. It builds up. And fast.
Studies show NSAIDs can reduce lithium clearance by 25% to 60%. That’s not a small change. It’s enough to send your lithium levels from a safe 0.6 mmol/L to a toxic 1.5 mmol/L or higher. The worst offenders? Indomethacin and piroxicam. Even common ones like ibuprofen can spike levels by 20-30%. Aspirin and celecoxib are less risky, but still not safe if you’re already at risk.
Why Your Kidneys Are the First to Suffer
Lithium doesn’t just sit in your blood-it directly damages kidney cells. It blocks an enzyme called GSK-3β, which leads to toxic buildup inside kidney tubules. NSAIDs make this worse by starving those same cells of blood flow. It’s a one-two punch: lithium weakens the cells, NSAIDs cut off their oxygen. The result? Acute kidney injury (AKI). A 2023 study found people taking both drugs had over three times the risk of AKI compared to those on lithium alone. And the highest risk? The first 30 days after starting an NSAID.
Long-term? It’s even scarier. Over five years, lithium users who took NSAIDs regularly had nearly three times the rate of permanent kidney damage-measured by a 30% drop in eGFR (a key kidney function number). For someone with already reduced kidney function (eGFR under 60), the risk jumps exponentially. This isn’t theoretical. In one study of 478 nephrology clinics, nearly 4 out of 10 cases of lithium-related kidney failure were directly tied to NSAID use.
Who’s Most at Risk-and Why It’s Often Missed
Age is the biggest silent factor. Over half of lithium-NSAID related kidney injuries happen in people over 65. Why? Kidneys naturally lose function as we age. A 70-year-old might have an eGFR of 55-just below normal-and think they’re fine. Then they take ibuprofen for a bad back. Within days, their lithium level spikes. They get dizzy, confused, shaky. They end up in the ER. By then, some have already lost 40% of their kidney function.
Another big problem? Communication gaps. A 2023 survey found only 58% of primary care doctors knew NSAIDs were dangerous with lithium. Patients often get NSAIDs from orthopedists, ER doctors, or pharmacists-not their psychiatrist. One Reddit thread had 127 users sharing stories of severe toxicity. Most said they were never warned. Twenty-nine were hospitalized. Sixteen developed permanent damage.
What You Should Do Instead
You don’t have to suffer in pain. But you need a safer plan.
- Acetaminophen (Tylenol) is your first choice. It doesn’t affect lithium levels. But don’t go over 3,000 mg a day-too much can hurt your liver.
- Tramadol is a second-line option. It’s an opioid-like painkiller with a low risk of lithium interaction. Start low (25 mg daily) and increase slowly.
- NSAIDs? Only if absolutely necessary. If you must take one-say, for a flare-up of severe arthritis-use the lowest dose for the shortest time possible. Never more than 7 days. Drink at least 3 liters of water daily. Get your lithium level checked 48-72 hours after starting it.
And here’s the hard truth: even after you stop the NSAID, the risk doesn’t vanish. It takes 7 to 10 days for your kidneys to fully recover their ability to clear lithium. So if you took naproxen for a week, you still need to monitor your levels for another week after you stop.
What Your Doctor Should Be Doing
Good care means more than just writing prescriptions. It means vigilance.
- Before starting an NSAID, check your lithium level. Do it again 48-72 hours after starting.
- Monitor your kidney function (creatinine and eGFR) weekly for the first month.
- Reduce your lithium dose by 25-50% if you’re on a high-risk NSAID like indomethacin.
- Document the risk clearly in your chart and give you a written warning.
Yet, a 2021 audit found only 62% of lithium-prescribing doctors included NSAID warnings in patient education materials. Compare that to 99% who warned about diuretics-another known lithium risk. That gap is deadly.

The Bigger Picture: Why This Keeps Happening
This isn’t just about one bad interaction. It’s about how our system fails patients. Electronic health records have alerts for lithium-NSAID interactions, but they’re soft warnings. Doctors can click past them. In 2023, over 28% of lithium users still got at least one NSAID prescription. That number jumps to 48% for patients seeing three or more doctors.
Some health systems are fixing this. Kaiser Permanente cut co-prescribing by more than half using mandatory education and hard EHR blocks. The VA? Only a 15% improvement. The difference? Enforcement.
The FDA now requires a boxed warning on lithium labels about NSAIDs. The European Medicines Agency is pushing for hard stops in prescribing systems. But until every doctor, pharmacist, and patient understands the danger, people will keep getting hurt.
What’s Next? New Hope on the Horizon
There’s promising research. A 2023 clinical trial tested a new drug that mimics kidney-protecting prostaglandins without interfering with lithium clearance. Early results showed an 87% drop in lithium level spikes. It’s not available yet, but it’s a sign that scientists are finally tackling this problem head-on.
Meanwhile, more people are switching to alternatives like valproate or lamotrigine. But lithium still has one unbeatable advantage: it cuts suicide risk by 44%. That’s higher than any other mood stabilizer. So for many, it’s not about giving up lithium-it’s about learning how to use it safely.
If you’re on lithium, your pain matters. But so does your kidney health. Don’t assume a common painkiller is harmless. Ask your doctor: "Is this safe with my lithium?" If they hesitate, get a second opinion. Your life depends on knowing the difference between a quick fix and a hidden threat.
Can I take ibuprofen with lithium?
No, it’s not safe. Ibuprofen can increase lithium levels by 20-30%, raising your risk of toxicity. Even short-term use can cause dizziness, confusion, tremors, or kidney damage. If you need pain relief, use acetaminophen instead. If ibuprofen is absolutely necessary, get your lithium level checked within 72 hours and drink plenty of water.
How long does the lithium-NSAID interaction last?
The interaction doesn’t end when you stop the NSAID. It can take 7 to 10 days for your kidneys to fully recover their ability to clear lithium. During that time, your lithium levels may still be higher than normal. Continue monitoring for symptoms and follow your doctor’s advice on blood tests.
What are the signs of lithium toxicity?
Early signs include nausea, vomiting, diarrhea, hand tremors, and increased thirst or urination. More serious symptoms include muscle weakness, confusion, slurred speech, dizziness, seizures, and irregular heartbeat. If you experience any of these while taking NSAIDs, stop the NSAID immediately and seek medical help. Lithium toxicity can be life-threatening.
Is celecoxib (Celebrex) safe with lithium?
Celecoxib is one of the safer NSAIDs for lithium users, but it’s not risk-free. It can still raise lithium levels by 10-15%, especially if you have reduced kidney function. It should only be used short-term and with close monitoring. Never assume it’s completely safe-always check your lithium levels before and after use.
Can NSAIDs cause permanent kidney damage with lithium?
Yes. Studies show that repeated or even single episodes of NSAID use in lithium patients can lead to permanent kidney damage, defined as a 40% or greater drop in eGFR. This damage is often irreversible. The risk is highest in older adults, those with preexisting kidney disease, and people who take NSAIDs regularly without monitoring.
What pain relievers are safe with lithium?
Acetaminophen (Tylenol) is the safest option and has no known interaction with lithium. Tramadol is a second choice and may be used cautiously under supervision. Avoid all NSAIDs-including aspirin, naproxen, diclofenac, and meloxicam-unless under strict medical supervision. Physical therapy, heat/cold therapy, and non-drug pain management should be explored first.

Comments
This is the kind of post that saves lives. I’ve seen too many people in my family get wrecked by 'harmless' ibuprofen while on lithium. My uncle ended up in the ER with confusion and kidney failure-all because his ortho gave him naproxen without checking his meds. If you’re on lithium, treat NSAIDs like poison. Because they are.
OMG YES. My mom took Advil for her knee for 3 days and went from fine to slurring words and vomiting. They didn’t even test her lithium levels until she was in the ICU. Why is this not on every NSAID bottle? Like, at least a big red warning? We’re not dumb, we just don’t know until it’s too late.
Let me be blunt: if your doctor doesn’t immediately flag NSAIDs with lithium, they’re not doing their job. This isn’t a 'maybe be careful' situation-it’s a 'you could die if you ignore this' scenario. And the fact that 40% of lithium-related kidney failures are tied to NSAIDs? That’s medical malpractice waiting to happen. I’ve seen it. I’ve documented it. I’ve screamed about it in forums. And still, people get prescribed it like it’s aspirin. It’s not. It’s a grenade with the pin pulled.
Acetaminophen? Fine. Tramadol? Maybe, if you’re desperate. NSAIDs? No. Not even 'just once.' Your kidneys aren’t replaceable. Your brain isn’t either. Stop normalizing this.
And yes, I’m mad. I should be. I lost a friend to this. She was 68. Thought she was being 'responsible' by taking a little Aleve for her arthritis. Four days later, she was in a coma. The ER doc said her lithium level was 2.1. Normal is 0.6 to 1.2. She never woke up.
Stop. Reading. This. And. Going. To. The. Pharmacy. Without. Asking. First.
I appreciate how detailed this is. I’m a nurse, and I’ve had patients come in confused because their PCP gave them ibuprofen without consulting their psychiatrist. It’s not just about the interaction-it’s about communication breakdowns across specialties. We need better systems. Not just warnings, but mandatory alerts that pop up and can’t be ignored. And maybe a simple handout given to every patient on lithium: 'If it’s an NSAID, don’t take it. Period.' Simple. Clear. Life-saving.
my dad’s on lithium and he swears by tylenol. he also does yoga and heat packs for his back. no more ibuprofen. no more risk. he says it’s worth it. i think he’s right.
It is profoundly irresponsible that this interaction remains so poorly understood by the medical community. The FDA’s boxed warning is a start, but it is woefully insufficient. The absence of mandatory, hard-stop EHR protocols constitutes a systemic failure of duty of care. One must question the ethical integrity of a healthcare infrastructure that permits such preventable iatrogenic harm to persist at scale. The data are unequivocal. The cost of inaction is measured in renal failure, psychiatric decompensation, and death. This is not merely a pharmacological issue-it is a moral imperative.
Based on the 2023 multicenter nephrology audit (n=478), the odds ratio for acute kidney injury (AKI) in lithium-NSAID co-administration was 3.2 (95% CI: 2.1–4.9), p<0.001. Furthermore, longitudinal eGFR decline ≥30% over 5 years was observed in 28.7% of NSAID-exposed patients versus 9.1% in controls (HR=3.04, p<0.01). The pharmacokinetic mechanism involves COX-1/2 inhibition → reduced renal prostaglandin synthesis → afferent arteriolar vasoconstriction → decreased GFR → impaired lithium excretion. The half-life of lithium clearance recovery post-NSAID discontinuation is approximately 8.3 days (95% CI: 7.1–9.5). Clinically, this necessitates serial lithium level monitoring at 48, 72, and 168 hours post-exposure.
I just want to say thank you for writing this. My sister’s been on lithium for 12 years. We never knew this risk until she got sick last year. Now we’re educating everyone we know. I’ve sent this to my dad’s doctor, my cousin’s pharmacist, even my cousin’s yoga instructor who was recommending turmeric capsules (which, I learned, can also interact). This isn’t just medical advice-it’s family safety. I’m so glad someone finally said it clearly.
Wow. Just… wow. I’m crying. I took naproxen for a week last year after my surgery. I didn’t tell my psych doctor. I thought it was fine. I got dizzy, my hands shook, I thought I was having a breakdown. Turns out, my lithium was 1.8. I spent 4 days in the hospital. I still have mild kidney damage. I’m 32. I shouldn’t be here. I should’ve known. I didn’t. And now I feel so guilty. Everyone needs to read this. Please. Please. Please.
i’m from india and my cousin is on lithium here. she asked me about painkillers and i googled it and found this post. i printed it out and gave it to her doctor. he didn’t know either. now he’s changed his practice. thank you for making this so clear. sometimes the most dangerous things are the ones we think are harmless.