When you pick up a new prescription, the pharmacist hands you a small paper-sometimes folded, sometimes stapled. It’s not just a receipt or a reminder. It’s a Medication Guide. And if you skip it, you could be missing life-saving information.
These guides aren’t optional. The FDA requires them for over 150 medications that carry serious, preventable risks. From blood thinners to antidepressants to cancer drugs, these guides tell you exactly what to watch for, when to get tested, and when to call your doctor. But most people don’t read them. A 2023 study found only 38% of patients consistently review their Medication Guides. That’s not because they’re careless-it’s because they’re confusing.
What’s in a Medication Guide (and why it matters)
Every Medication Guide follows the same seven-section format, designed to cut through medical jargon. The FDA mandates they be written at a 6th-8th grade reading level, with bold headers and a minimum 10-point font. That’s not random-it’s because people need to understand this quickly, especially when they’re stressed or new to a drug.
Take warfarin (Coumadin), a blood thinner. Its guide doesn’t say, “May cause bleeding.” It says: “If you notice unusual bruising or bleeding that lasts a long time, call your doctor right away.” It tells you to get your INR tested at least once a month-and more often if your dose changes. No guessing. No vague warnings. Just clear, actionable steps.
Antidepressants like sertraline or fluoxetine have similar clarity. The guide says: “Pay close attention to any changes, especially sudden changes, in mood, behavior, thoughts, or feelings.” And it adds: “This is very important when an antidepressant is started or when the dose is changed.” That’s not just advice-it’s a warning tied to a specific time window. The highest risk isn’t after months of use. It’s in the first 4 to 6 weeks.
Find the most important part first
Don’t start at the top. Go straight to the section titled: “What is the most important information I should know about [drug name]?”
This is where the FDA forces manufacturers to highlight the deadliest risks in plain language. For clozapine (Clozaril), used for treatment-resistant schizophrenia, it says: “About 1 in 200 people taking clozapine may develop a condition called agranulocytosis.” That’s not “possible.” That’s “1 in 200.” And it doesn’t stop there. It adds: “You’ll need weekly blood tests for the first 6 months.”
That’s the pattern. The most important section doesn’t sugarcoat. It doesn’t say “rare side effects.” It gives numbers. It gives timing. It gives consequences. If you remember nothing else, remember this: the most important section is the one that tells you what could kill you-and how to stop it.
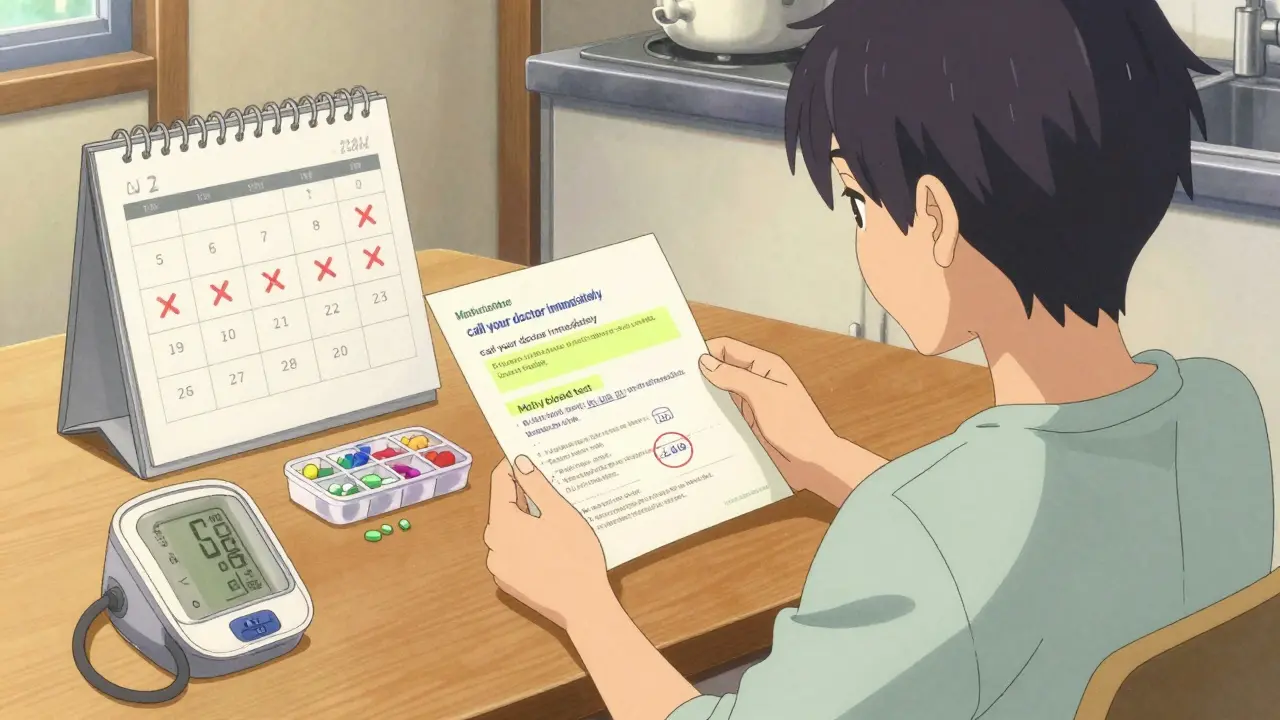
Connect the dots between side effects and monitoring
Here’s where most people get lost. They read the list of side effects, then close the guide. But the real power is in linking what you’re told to watch for with when you’re supposed to get checked.
Look at tofacitinib (Xeljanz), a JAK inhibitor for rheumatoid arthritis. The guide says: “Serious side effects include changes in blood cell counts.” Then, in the “How should I take this medicine?” section, it says: “Your healthcare provider should perform blood tests before you start and every 3 months while taking this medicine.”
That’s the connection. The side effect isn’t just something to worry about-it’s something you’re supposed to catch early. And the guide tells you exactly how often to get tested. No interpretation needed.
Same with abiraterone (Zytiga), used for prostate cancer: “Blood tests before you start and every month after.” If you miss one, you’re flying blind.
Pro tip: When you get your guide, highlight every word that says: test, monitor, check, measure, blood, lab, INR, CBC. Circle every time frame: weekly, monthly, every 3 months, before starting, after 2 weeks. Underline every symptom that says: call your doctor immediately. You’re not reading-you’re mapping.

Watch out for the red flags
The Agency for Healthcare Research and Quality (AHRQ) identified seven phrases that should trigger immediate attention. If you see any of these, stop and think:
- “Get blood tests regularly”
- “Call your doctor immediately if…”
- “Do not stop taking without talking to your doctor”
- “Avoid sunlight exposure”
- “Do not drink alcohol”
- “May impair driving ability”
- “Keep all scheduled appointments”
These aren’t suggestions. They’re safety checkpoints. For example, if your guide says “avoid sunlight,” it’s probably because the drug makes your skin burn faster-or even cause skin cancer. That’s not a minor warning. It’s a daily habit change.
And “do not stop taking without talking to your doctor”? That’s often for drugs like antidepressants or seizure medications. Stopping cold turkey can cause seizures, extreme anxiety, or even death. The guide isn’t being dramatic. It’s being precise.
What to do if your guide is missing
By law, a Medication Guide must be given to you every time you fill your prescription. But a 2022 audit found 41% of independent pharmacies didn’t always hand them out.
If you don’t get one, ask for it. Say: “I need the Medication Guide for this drug.” If they say they don’t have it, ask for the FDA’s online version. Go to DailyMed (dailymed.nlm.nih.gov), search your drug name, and download the latest guide. Print it. Bring it to your next appointment.
Some pharmacies now offer QR codes on the bottle that link directly to the current guide. Pfizer and other big manufacturers started this in 2023 for high-risk drugs like cancer treatments. If your bottle has one, scan it. It’s faster than reading a paper copy.
Use the 3-2-1 method to stay safe
Reading the guide once isn’t enough. Risks change. New warnings come out. The FDA requires manufacturers to update guides within 30 days of new safety info-and 92% did so in 2022.
Here’s how to keep up:
- 3 minutes before your first dose - Read the whole guide. Highlight the key parts.
- 2 minutes before each refill - Check if the guide has changed. Look for new warnings or updated testing schedules.
- 1 minute during treatment - When you feel something off, reread the “Serious Side Effects” section. Is what you’re feeling listed? Is there a monitoring step you missed?
A 2022 University of Michigan study found patients who used this method had 68% fewer adverse events. Why? Because they weren’t guessing. They were following a plan.
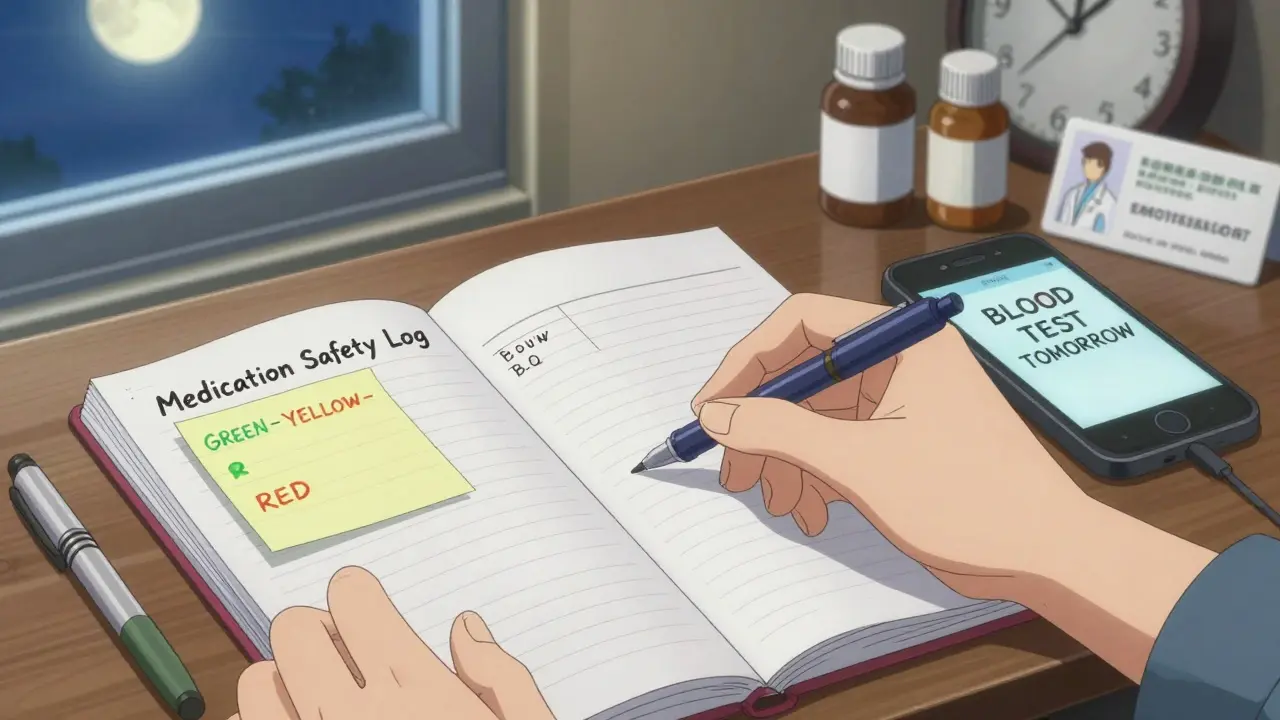
Track your monitoring like a pro
For drugs that need blood tests-like warfarin, clozapine, or tofacitinib-create a simple calendar. Write down:
- When your next test is due
- What test it is (INR, CBC, liver enzymes)
- Who to call if you miss it
Put it on your fridge. Set a phone reminder. Some patients use a small notebook labeled “My Medication Safety Log.” Others use free apps like Medisafe or MyTherapy. The goal isn’t to be perfect-it’s to never miss a test because you forgot.
Pharmacist Sarah Chen in Birmingham says: “When I physically point out the monitoring section and explain it takes less than 90 seconds to read, compliance jumps from 45% to 82%.” You don’t need to be a doctor. You just need to pay attention for 90 seconds.
What if you still don’t understand?
Even with plain language, some guides are still hard to read. That’s why 63% of patients misunderstand time-sensitive instructions. They think “monitor monthly” means “watch for symptoms.” But it means “get a blood test every 30 days.”
Don’t guess. Ask. Bring your guide to your doctor or pharmacist and say: “I want to make sure I’m doing this right. Can you help me understand what I need to watch for and when?”
There’s no shame in asking. The guides exist because these drugs are powerful-and risky. The system works only if you use it.
And if you’re on a high-risk drug-like an anticoagulant, immunosuppressant, or psychiatric medication-consider asking for a “traffic light” system. Green: normal. Yellow: call your provider. Red: go to the ER. Write it on your guide. Stick it on your mirror. Make it visual.
Because the difference between reading a Medication Guide and ignoring it isn’t just about safety. It’s about control. You’re not just taking a pill. You’re managing a risk. And you have the right-and the tool-to do it right.

Comments
I used to skip these guides too until my mom had a bad reaction to warfarin. Now I read every single one like it’s a survival manual. Seriously, 90 seconds could save your life.
Let’s be real-the FDA’s ‘plain language’ is just corporate legalese with fewer semicolons. The real issue is pharmaceutical capitalism weaponizing patient ignorance. These guides are performative compliance, not genuine harm reduction. The system isn’t broken-it’s designed this way.
This is the most useful thing I’ve read all year. I’m printing this out and taping it to my medicine cabinet. Thank you.
Wait… so you’re telling me the government and Big Pharma are forcing you to read this… but only 38% do? That’s not negligence-that’s a cover-up. They WANT you to miss the warnings. They profit from your hospital stays. I’ve seen the memos. They track which patients ignore the guides and target them for higher-dose trials. You’re not just reading a paper-you’re fighting a system.
Wow. So the solution to pharmaceutical risk is… reading? I’m shocked. Next you’ll tell me wearing seatbelts reduces car crash fatalities.
USA think they invented safety! 😂 In Nigeria, we just ask the pharmacist: ‘This thing gonna kill me?’ He laughs, says ‘Maybe, but your pain worse.’ We don’t need 7-section guides-we need trust. And maybe less paperwork. 🤷♀️💊
I love how you broke this down. My grandma used to say, ‘If it’s important, they’ll say it twice.’ Turns out, the guide says it once-but in bold. I’m starting the 3-2-1 method tomorrow.
Scan the QR code. Read the guide. Don’t die. Simple.
Oh honey, I read these like fashion magazines. Highlighted the ‘call your doctor’ parts in neon pink. My therapist says I have a ‘hyper-vigilant health aesthetic.’ I call it self-care with flair. 💅🩺
THIS. IS. A. GAME. CHANGER. 🚨 I almost missed my monthly blood test last month because I was ‘too busy.’ Now I’ve got a little alarm that goes off at 7 a.m. every 30 days. I even made a TikTok about it. 12K likes. People are crying. This is important. 🫶
Let me guess-you think reading a 12-page PDF makes you ‘informed.’ Meanwhile, real doctors are prescribing meds based on algorithms and kickbacks. You’re optimizing the wrong thing. Knowledge is power? Nah. Power is knowing who to bribe to get the updated guide before the FDA releases it.
Man, I’ve been there. Took me three years to realize my anxiety meds needed monthly liver checks. I missed two. Ended up in the ER. This guide? It’s not advice-it’s your lifeline. Start small. One section a day. You got this.
My husband is on clozapine. We use the ‘traffic light’ system you mentioned. Green = good. Yellow = call the nurse. Red = go to ER. We printed it, laminated it, and put it on the fridge next to the grocery list. It’s saved us twice already. Thank you for making this so clear.
As someone who’s read every FDA guideline since 2008, I must say: this is the most coherent summary I’ve seen. The ‘3-2-1’ method? Genius. The fact that you didn’t mention the 2019 EMA revision on INR thresholds, though… is concerning. But still-bravo.
Just shared this with my sister who’s on Xeljanz. She didn’t even know she needed blood tests every 3 months. She’s scheduling hers now. This post might’ve saved her life. Seriously, thank you.