For many people, type 2 diabetes doesn’t come with a siren. No sudden collapse, no emergency room rush. Instead, it creeps in quietly-fatigue that won’t lift, thirst that won’t quit, wounds that take forever to heal. By the time it’s diagnosed, the damage may already be spreading through nerves, kidneys, and blood vessels. The good news? You can stop it. Not always reverse it, but definitely control it-before it controls you.
What Actually Happens in Type 2 Diabetes?
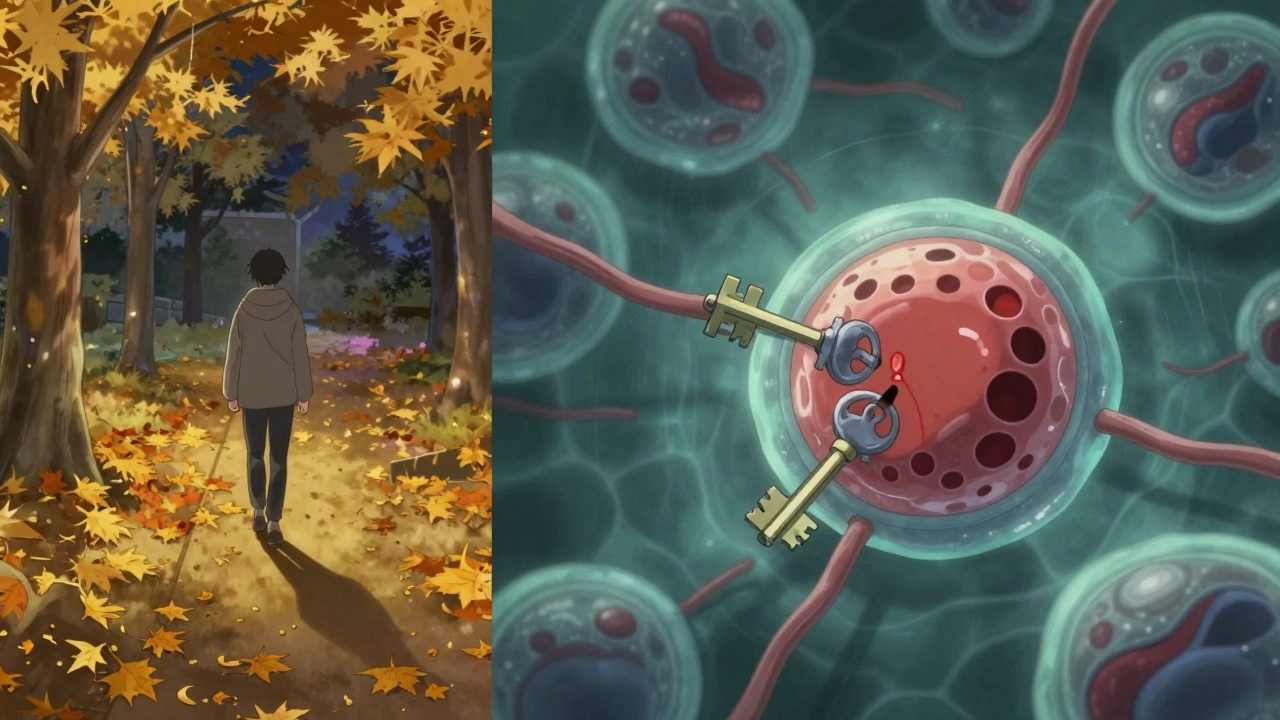
Your body runs on glucose, the sugar from food. Insulin, a hormone made by your pancreas, acts like a key, unlocking cells so glucose can enter and be used for energy. In type 2 diabetes, that key stops working properly. First, your cells become resistant to insulin. They don’t listen. So your pancreas works harder, pumping out more insulin to force glucose in. For years, it keeps up. But eventually, the pancreas gets tired. It can’t produce enough insulin anymore. Glucose piles up in your blood instead of powering your muscles and brain. That’s high blood sugar-and that’s type 2 diabetes.
It’s not just about eating too much sugar. It’s about your body’s long-term response to excess weight, inactivity, and genetics. Around 80-90% of people with type 2 diabetes have insulin resistance before diagnosis. The pancreas compensates by making 2-3 times the normal amount of insulin. But that’s like revving an engine until it burns out.
What Are the Real Symptoms?
Most people don’t feel like they’re sick. That’s why nearly 1 in 4 Americans with diabetes don’t even know they have it. Symptoms build slowly. You might write them off as stress, aging, or just being tired.
- Constant thirst-you’re drinking more water than ever, but still feel dry.
- Frequent urination-your bladder’s on overdrive because your kidneys are trying to flush out extra sugar.
- Unexplained weight loss-even if you’re eating normally, your body can’t use glucose for fuel, so it starts breaking down muscle and fat.
- Extreme fatigue-your cells are starving for energy, even though there’s plenty of sugar in your blood.
- Blurred vision-high glucose swells the lenses in your eyes, making focus hard.
- Slow-healing cuts or sores-high sugar damages blood vessels and weakens your immune response.
- Recurrent infections-yeast infections, urinary tract infections, or skin boils that won’t go away.
- Numbness or tingling-especially in hands and feet. This is nerve damage from prolonged high blood sugar.
- Dark, velvety patches-on your neck, armpits, or groin. This is called acanthosis nigricans and is a clear sign of insulin resistance.
Some people have none of these. Their diabetes is found during a routine blood test. That’s why getting checked-especially if you’re overweight, over 45, or have a family history-isn’t optional. It’s essential.
Why Did This Happen to Me?
Blaming yourself doesn’t help. Type 2 diabetes isn’t a failure of willpower. It’s a mix of biology and environment.
Obesity is the biggest trigger. If your BMI is over 30, your risk is 80 times higher than someone with a BMI under 22. Fat tissue, especially around the belly, releases chemicals that make your body resistant to insulin.
Inactivity makes it worse. Muscle uses glucose. If you’re sitting most of the day, your muscles don’t need sugar, so your body doesn’t respond to insulin well. Just 30 minutes of walking a day cuts your risk by 30%.
Genetics play a huge role. If one of your parents has type 2 diabetes, your risk jumps by 40%. If both do, it’s even higher. Over 400 genes have been linked to the condition. Some affect how your body stores fat, others how your pancreas makes insulin.
Ethnicity matters too. Native Americans, African Americans, Hispanic/Latino Americans, and Asian Americans have higher rates than non-Hispanic White Americans. It’s not race-it’s biology shaped by history, diet, and access to care.
Aging increases risk. After 45, your body becomes less efficient at using insulin. But now, children and teens are getting it too. In the U.S., over 287,000 people under 20 have type 2 diabetes-up sharply in the last decade.
What Happens If You Ignore It?
High blood sugar doesn’t just make you tired. It quietly damages your body.
Heart disease is the #1 killer. People with type 2 diabetes are 2-4 times more likely to have a heart attack or stroke. In fact, 65-80% of deaths among diabetics are from cardiovascular problems.
Nerve damage (neuropathy) affects 60-70% of people after 10 years. It starts with tingling in the feet. Left unchecked, it leads to pain, loss of sensation, and ulcers. One in five of those ulcers ends in amputation.
Kidney failure is common. Type 2 diabetes causes 44% of all new cases of kidney failure requiring dialysis. Your kidneys filter blood. High sugar clogs them.
Eye damage (retinopathy) blinds 17,000 Americans every year. It’s often preventable with regular eye checks.
Brain health is at risk too. People with diabetes have a 2-3 times higher risk of Alzheimer’s. Some scientists even call it “type 3 diabetes” because insulin resistance in the brain may play a role.
Mental health takes a hit. Depression is twice as common in people with diabetes-and it makes blood sugar harder to control. It’s a cycle: high sugar makes you feel awful, feeling awful makes you less likely to manage it, and it gets worse.
How Do You Actually Manage It?
Management isn’t about perfection. It’s about consistency.
1. Lifestyle is the foundation. The CDC’s National Diabetes Prevention Program proved that losing just 7% of your body weight and walking 150 minutes a week cuts your risk of developing diabetes by 58%. That’s more effective than most medications.
Start small. Swap soda for water. Take the stairs. Walk after dinner. You don’t need a gym membership. You need movement.
2. Medication isn’t failure-it’s support. Metformin is the first-line drug. It’s cheap, safe, and reduces HbA1c by 1-2%. It doesn’t cause weight gain or low blood sugar. Many people stay on it for life.
If metformin isn’t enough, newer drugs like GLP-1 agonists (semaglutide, liraglutide) or SGLT2 inhibitors (empagliflozin, dapagliflozin) are now preferred. They don’t just lower sugar-they protect your heart and kidneys, and help you lose weight. Some people lose 10-15 pounds without trying.
3. Monitor your numbers. HbA1c measures your average blood sugar over 3 months. Most people aim for under 7%. But if you’re older or have other health issues, your doctor might set a higher target (7-8%) to avoid dangerous lows.
Continuous glucose monitors (CGMs) are no longer just for type 1. Medicare now covers them for type 2 patients who need insulin. Even if you’re not on insulin, a CGM can show you how food, sleep, and stress affect your sugar. It’s eye-opening.
4. Sleep and stress matter. Poor sleep raises cortisol, which raises blood sugar. Chronic stress does the same. If you’re not sleeping well or you’re always wound up, your diabetes will be harder to control-even if you’re eating right.

Can Type 2 Diabetes Be Reversed?
“Reversed” doesn’t mean cured. It means your blood sugar is normal without medication. And yes, it’s possible.
The DiRECT trial in the UK showed that 46% of people with type 2 diabetes for less than 6 years achieved remission after a year of a very low-calorie diet (800-850 calories/day for 3-5 months), followed by gradual food reintroduction and ongoing support. They lost an average of 15 kg. Their pancreas started making insulin again.
It’s not easy. But it’s not magic. It’s weight loss-enough to reduce fat around the liver and pancreas. That’s what restores insulin function.
Even if you don’t lose 15 kg, losing 5-10% of your body weight can dramatically improve your blood sugar, reduce meds, and lower your risk of complications.
What’s New in Treatment?
Medicine is moving fast.
Tirzepatide (Mounjaro), a dual GIP/GLP-1 agonist, was approved in 2022. It lowers HbA1c by up to 2.3% and helps people lose 11-15 pounds. It’s now being studied for use in non-diabetic obesity.
Hybrid closed-loop systems (like the MiniMed 780G) are now approved for type 2 diabetes. These are “artificial pancreas” devices that adjust insulin automatically based on real-time glucose readings. They’re not for everyone-but if you’re on multiple daily insulin shots, they can cut your stress and improve control.
Research like the All of Us program is trying to understand why diabetes hits some groups harder than others. The goal? Personalized prevention based on your genes, environment, and lifestyle-not a one-size-fits-all approach.
Where Do You Start Today?
Don’t wait for symptoms. If you’re overweight, inactive, over 45, or have a family history, get your blood sugar checked. A simple fasting glucose test or HbA1c test takes five minutes.
If you’ve just been diagnosed: breathe. This isn’t the end. It’s a wake-up call-and you have more power than you think.
Start with one change. Walk 20 minutes after dinner. Swap one sugary drink for water. Talk to your doctor about metformin. Don’t try to fix everything at once.
And remember: you’re not alone. Over 500 million people worldwide live with type 2 diabetes. Many of them are managing it well. So can you.
Can type 2 diabetes be cured completely?
Type 2 diabetes can’t be cured like an infection, but it can go into remission. That means blood sugar levels return to normal without medication. This usually happens after significant weight loss-often 10% or more of body weight. The pancreas regains its ability to produce insulin. But if weight is regained, diabetes can return. Remission isn’t permanent unless lifestyle changes stick.
Do I need to take insulin if I have type 2 diabetes?
Not at first. Most people start with lifestyle changes and oral medications like metformin. Over time, as the pancreas loses insulin production, insulin therapy may become necessary. About 30% of people with type 2 diabetes eventually need insulin. It’s not a failure-it’s part of the disease’s natural progression. Many people use insulin for a short time to reset their system, then switch back to pills.
Can I still eat sugar if I have type 2 diabetes?
Yes-but in moderation. You don’t need to eliminate sugar entirely. The issue isn’t sugar alone-it’s total carbohydrate intake and how it affects your blood sugar. A small piece of cake occasionally won’t ruin your progress. What matters more is avoiding sugary drinks, processed snacks, and refined carbs like white bread and pastries. Focus on whole foods: vegetables, lean protein, healthy fats, and whole grains.
How often should I check my blood sugar?
It depends. If you’re on insulin or taking medications that can cause low blood sugar, your doctor may ask you to check daily. If you’re managing with diet and metformin, checking once or twice a week might be enough. HbA1c tests every 3-6 months give you the big picture. Continuous glucose monitors (CGMs) are becoming more common-they show trends, not just numbers, which helps you see how food, sleep, and stress affect you.
Is type 2 diabetes hereditary?
Yes, genetics play a big role. If one parent has type 2 diabetes, your risk is about 40%. If both do, it’s higher. But genes aren’t destiny. Even if you have a strong family history, you can delay or prevent diabetes with healthy habits. The Diabetes Prevention Program showed that lifestyle changes cut risk by 58%-even in people with the highest genetic risk.
Can weight loss surgery help type 2 diabetes?
Yes, for people with obesity (BMI over 35), weight loss surgery (like gastric bypass or sleeve gastrectomy) can lead to diabetes remission in up to 80% of cases. It’s not just about losing weight-the surgery changes gut hormones that improve insulin sensitivity. It’s a powerful tool, but it’s not for everyone. It requires lifelong dietary changes and medical follow-up.
What’s the biggest mistake people make managing type 2 diabetes?
Waiting until something goes wrong. Many people wait until they have nerve pain, vision problems, or kidney issues before making changes. By then, damage is already done. The best time to act is right after diagnosis. Early, consistent management-even small changes-can prevent complications for decades. Don’t wait for a crisis. Start today.
If you’re struggling, find support. Join a diabetes education class. Talk to a dietitian. Connect with others online or in person. You don’t have to do this alone. And remember-managing type 2 diabetes isn’t about being perfect. It’s about showing up, day after day, and choosing your health-even when it’s hard.


Comments
It’s not about willpower. It’s about biology. Your body isn’t broken-it’s adapting to a world that never asked if it could keep up.
Genes load the gun. Environment pulls the trigger. And now we’re surprised when the shot rings out?
We treat diabetes like a personal failure when it’s a systemic collapse.
Stop blaming the patient. Start blaming the food system.
The real disease isn’t insulin resistance-it’s capitalism.
And yeah, I know that sounds dramatic. But when your town has three fast food joints and one grocery store with expired kale… what else is there to say?
Lmao another woke medical essay. Just eat less sugar and move your ass. No one cares about your genetics or your trauma. If you’re fat and tired it’s because you’re lazy. End of story.
Heyyyy I just wanna say-you’re not alone 💪
My cousin was diagnosed last year and started walking after dinner with his dog. Lost 12 lbs in 3 months. No meds. Just consistency.
And guess what? He says he feels like a new person.
You don’t have to be perfect. Just show up.
Even a 10-minute walk counts. Even swapping soda for sparkling water counts.
You got this. I believe in you. 🌱❤️
One must consider the epistemological framework underlying the notion of 'reversal' in metabolic pathology.
Remission, as currently operationalized, is a statistical artifact of weight loss, not a biological restoration.
Insulin sensitivity may transiently improve, but the underlying epigenetic dysregulation persists.
One cannot 'cure' a polygenic disorder with caloric restriction alone.
Moreover, the DiRECT trial’s sample was highly selective-low socioeconomic status, high dropout rates, minimal long-term follow-up.
One wonders if this is medicine-or performative optimism dressed in clinical garb.
🫡
Okay but imagine if your body was a phone and insulin was the charger.
For years you keep plugging it in but the port’s clogged with sugar gunk.
Then one day-BAM-the charger just stops working.
That’s what happens.
And yeah, you can clean the port. You can get a new charger. You can even use a wireless pad.
But you gotta stop dumping sugar in the port every five minutes.
It’s not magic. It’s maintenance.
And honestly? You’re not broken. You’re just overdue for a system update. 💻📱
i just started checking my sugar with a cgms and holy moly it’s wild how much bread messes me up. like… i thought i was eating healthy. turns out i was just eating carbs in a fancy package. mind blown 🤯
Let’s be real-no one’s gonna lose 15kg unless they’re already rich, white, and have a personal trainer.
And don’t even get me started on ‘lifestyle changes’ when you work two jobs and your kid has asthma.
Meanwhile, Big Pharma is selling GLP-1s for $1,000 a month.
They want you to believe this is a personal problem.
It’s not. It’s a poverty problem wrapped in a lab coat.
And the people who wrote this article? They probably don’t even have to worry about food stamps.
So yeah. Keep preaching. I’ll be over here trying to afford insulin.
Meanwhile, my blood sugar’s just trying to survive.
OMG I JUST GOT DIAGNOSED LAST WEEK AND I’M SO SCARED 😭
BUT I’M STARTING TOMORROW-WALKING 20 MINUTES AFTER DINNER AND DRINKING WATER INSTEAD OF SODA.
IF I CAN DO IT, YOU CAN TOO.
YOU’RE NOT ALONE. I’M ROOTING FOR YOU. 🌟💖
AND YES I KNOW I USED TOO MANY EMOJIS BUT I MEAN IT.
Richard, you’re an idiot.
It’s not laziness. It’s systemic.
Try living in a food desert and then come talk to me about ‘just moving your ass.’
My grandma had diabetes, worked 60 hours a week, ate what she could afford-and still got blamed for it.
People like you make this harder for everyone else.
Go read a book. Or better yet-listen to someone who’s actually living it.
🙄
Oh look, another ‘you can reverse it!’ fairy tale.
Meanwhile, 30% of people end up on insulin anyway.
And 80% of those ‘remissions’? They’re back in 2 years.
They sell this like it’s a wellness influencer glow-up.
But the truth? It’s a slow death sentence with a fancy app.
And yes, I’m salty.
Because I’ve been doing this for 12 years.
And no, I didn’t ‘fail.’
The system did.