Your throat flares up, then your nose blocks. It eases, then swings back again. If you’re stuck in that loop, you’re not imagining it-the throat and sinuses share the same airway, germs, and drainage paths. This piece nails down how the two conditions feed off each other, how to tell them apart, and what actually stops the back‑and‑forth.
- They share plumbing: inflamed tonsils and swollen sinuses cross‑irritate via post‑nasal drip, mouth breathing, and shared germs.
- Most episodes are viral and settle in 3-7 days with comfort care; antibiotics help only a narrow slice.
- Use FeverPAIN (throat) and the “10 days or double‑worsening” rule (sinus) to judge if you need a prescription.
- Recurring bouts often ride on allergies, big adenoids, reflux, smoke exposure, or biofilm‑forming bacteria. Fixing those breaks the cycle.
- Seek urgent help for severe one‑sided throat pain with drooling/trismus, eye swelling/vision changes, very high fever, stiff neck, or confusion.
How tonsillitis and sinus infections fuel each other
The nose, sinuses, adenoids, and tonsils sit in one airway corridor. That shared space is why irritation in one spot so easily flips on the other. The key players:
- Post‑nasal drip: inflamed sinuses leak mucus that trickles over the tonsils. That drip carries inflammatory gunk and bacteria, making an already sore throat angrier.
- Mouth breathing: when your nose blocks, you mouth‑breathe. Dry air over the tonsils cracks the protective layer and stings the tissue, which then swells faster.
- Shared microbes: classic throat culprits (Group A Strep) and sinus regulars (Haemophilus, Moraxella, Staph) mingle in the nasopharynx. Once one area is inflamed, the other gets easier to colonise.
- Waldeyer’s ring: this lymphatic ring (tonsils, adenoids, other tissue) is one immune unit. Swollen adenoids can trap infection and keep seeding the sinuses and tonsils.
- Biofilms: in chronic cases, mixed bacteria form slimy communities that dodge antibiotics and linger on the tonsils/adenoids and sinus lining. That’s one reason symptoms keep relapsing.
What starts the dominoes? Often a cold or allergy flare. A viral upper‑respiratory infection swells the nasal lining, blocks sinus drainage, and ramps up mucus. That inflames the tonsils. Or a primary throat infection closes your nose reflexively, pushes you into mouth breathing, and the sinuses stall out.
Who’s more likely to bounce between both?
- Kids with large adenoids/tonsils or frequent colds at school.
- Adults with allergic rhinitis or hay fever (especially spring and late summer in the UK).
- People exposed to smoke or dry indoor air (think radiators in a British winter).
- Those with reflux, which can quietly irritate the throat, especially overnight.
- Chronic nasal septum deviation, nasal polyps, or narrow sinus openings.
Quick way to spot what’s on top today:
- Leaning throat: sudden sore throat, pain on swallowing, red/swollen tonsils (maybe with white patches), fever, tender neck glands, little to no cough. Use FeverPAIN to judge strep risk.
- Leaning sinus: facial pressure (worse when bending), blocked nose, thick nasal discharge, reduced smell, tooth pain, ear pressure.
- Both: sore throat plus heavy post‑nasal drip and nose blockage. Often viral or allergy‑driven.
Evidence you can trust: UK NICE guidance backs two simple decision tools. For sore throats, FeverPAIN helps decide who benefits from antibiotics (NICE NG84, updated 2024). For acute sinusitis, antibiotics rarely help before day 10 unless symptoms are severe; intranasal steroids and time do better (NICE NG79, updated 2024). ENT UK and NHS England’s Evidence‑Based Interventions also guide when to consider surgery for recurrent sore throats.
One more piece many people miss: adenoids. They sit behind the nose, especially prominent in children. Chronically infected adenoids can drip infected mucus down to the tonsils and into the sinuses. That’s why adenoidectomy, sometimes paired with tonsillectomy, can break repeat cycles in children with sleep apnoea or constant infections.
What to do now: step‑by‑step care, tests, and when to seek treatment
Here’s a clean plan to manage symptoms, avoid unnecessary antibiotics, and get the right help if you need it.
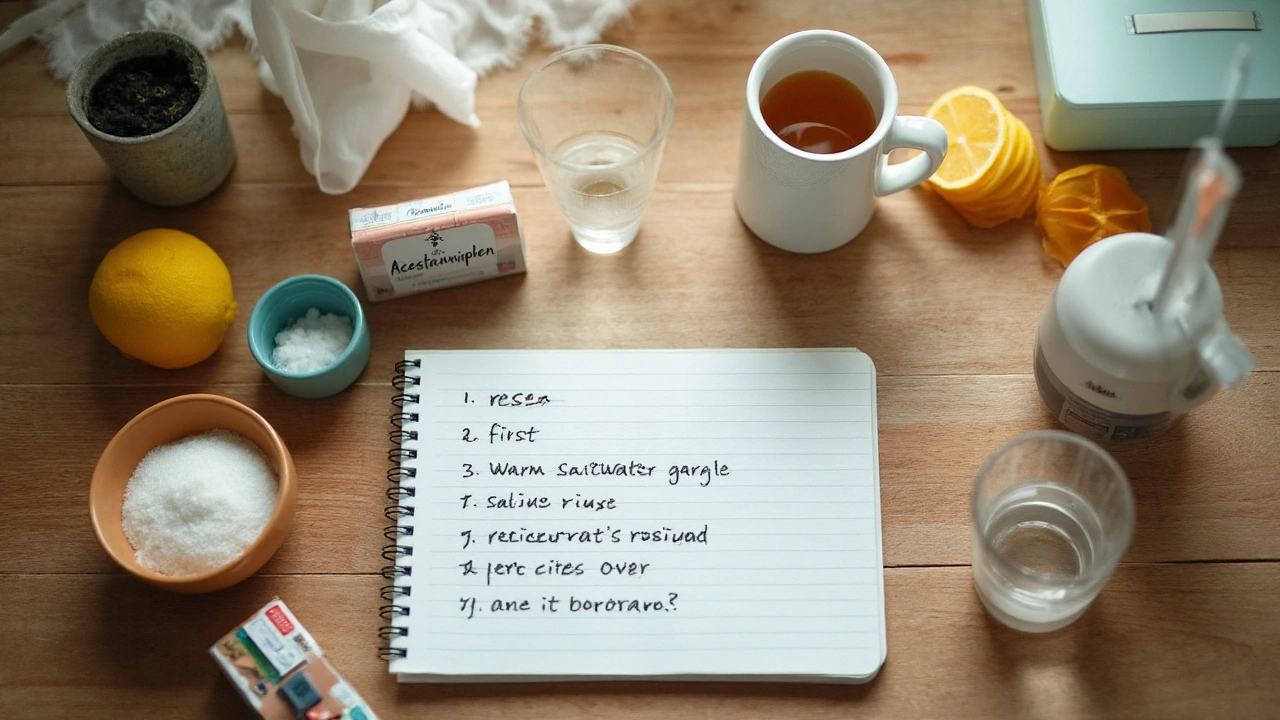
First 48-72 hours (most viral):
- Fluids and soft foods: warm soups, non‑acidic teas, ice lollies. It keeps mucus thin and swallowing less painful.
- Pain and fever relief: paracetamol or ibuprofen as per the label. They reduce inflammation in both the tonsils and sinus lining.
- Salt‑water gargles: half a teaspoon of table salt in a cup of warm water 3-4 times daily. Cheap, reduces throat swelling.
- Nasal care: saline spray or rinse once or twice a day. Cochrane reviews support saline to improve sinus symptoms and speed recovery.
- Intranasal steroid (e.g., beclometasone, fluticasone): if you have clear allergic triggers or significant nose blockage, a once‑daily steroid spray for 1-2 weeks can calm the sinuses and cut post‑nasal drip.
- Decongestant caution: short‑term nasal decongestant sprays can help for 2-3 days, but don’t push past that or you’ll rebound congest.
- Honey for cough and throat irritation: a spoon at night can soothe; avoid in children under one year.
- Sleep smart: head slightly raised, lie on your side if drip bothers you when flat.
- Air quality: avoid smoke and strong fragrances; a lukewarm shower or a bowl of steam can loosen thick mucus.
How to decide on antibiotics for a sore throat (adult and child):
- Use FeverPAIN (backed by NICE NG84): Fever in the last 24 hours, Pus on the tonsils, Attend within 3 days of symptoms, Inflammation/erythema of tonsils, No cough or coryza. One point each.
- 0-1 points: self‑care.
- 2-3 points: consider a delayed prescription (use only if not improving or worsening after 2-3 days).
- 4-5 points: consider immediate antibiotics or a rapid strep test where available.
- Typical first‑line in the UK: phenoxymethylpenicillin for 5-10 days; if allergic, clarithromycin (check interactions) or erythromycin in pregnancy. Your GP will tailor this.
How to decide on antibiotics for acute sinusitis:
- Time rule: most cases improve by day 10. If it’s under 10 days and not severe, prioritise nasal steroids, saline, rest, and pain relief.
- Double‑worsening or >10 days with persistent thick discharge, facial pain, or fever: that’s when a GP may consider antibiotics.
- First‑line UK options: amoxicillin for 5 days (if no penicillin allergy) or doxycycline; macrolide if appropriate. Nasal steroids often help more than antibiotics on their own.
When to see your GP, NHS 111, or urgent care:
- Severe throat pain on one side, trismus (can’t open mouth), hot potato voice, drooling: possible quinsy (peritonsillar abscess). Urgent same‑day assessment.
- Eye swelling, redness, severe pain with eye movements, reduced or double vision: possible orbital cellulitis from sinus infection. Emergency care.
- Very high fever, rash, dehydration, confusion, stiff neck, severe headache: get urgent help.
- Symptoms not settling by 10 days for sinusitis or 7 days for sore throat, or you keep bouncing back every few weeks.
- Breathing pauses at night, loud snoring, daytime sleepiness in a child: ENT review for enlarged tonsils/adenoids.
What about tests?
- Rapid strep tests: useful if FeverPAIN is high and you want to avoid unnecessary antibiotics. Some UK practices offer them.
- Swabs: rarely needed unless symptoms are severe, persistent, or unusual.
- Blood tests: not routine for simple cases.
- Scans: CT or MRI only if complications, severe recurrent disease, or pre‑surgery planning (per NICE).
Breaking the relapse cycle: fix the drivers
- Allergy plan: daily intranasal steroids during pollen season, non‑drowsy antihistamines when itchy/sneezy, and regular saline rinse. If symptoms are heavy every spring/summer, speak to your GP about an allergy referral.
- Reflux tactics: smaller evening meals, avoid late‑night eating, limit alcohol and acidic foods, prop the bedhead a touch. If classic heartburn or throat clearing is constant, ask about treatment.
- Hygiene: hand‑washing, don’t share cups, replace toothbrush 24-48 hours after starting antibiotics for strep throat.
- Environment: smoke‑free home, and gentle humidity helps noses behave better in winter.
- Fitness and rest: regular sleep and outdoor movement support immune recovery. You don’t need hero workouts-short walks work.
When does surgery enter the chat?
- Tonsillectomy: considered if sore throat episodes are severe and frequent-classically 7 or more in one year, 5 per year for 2 years, or 3 per year for 3 years-and they’re disabling and well‑documented. Also after a quinsy or with sleep apnoea. UK criteria follow NHS England’s Evidence‑Based Interventions and ENT UK guidance.
- Adenoidectomy (often in children): for nasal obstruction, recurrent glue ear, or chronic nasal infections. Sometimes paired with tonsillectomy if both drive problems.
- Sinus surgery: if medical treatment fails for chronic rhinosinusitis or polyps, or if complications develop. It aims to open drainage and reduce inflammation, not to “cure colds.”
Credible sources shaping this advice: NICE NG84 (acute sore throat) and NG79 (acute sinusitis), ENT UK recommendations on tonsillectomy thresholds, Cochrane reviews on saline irrigation and intranasal steroids, and BMJ updates on antibiotic stewardship up to 2024-2025.
Scenarios, checklists, and smart FAQs
Spot‑the‑difference checklist (quick self‑screen):
- Sudden high fever, bad swallowing pain, white spots, no cough: higher chance of bacterial throat infection. Use FeverPAIN.
- Facial pressure, blocked nose, thick discharge, poor smell: likely sinusitis.
- Allergy season, itchy eyes, clear runny nose, sneezing: allergic rhinitis flaring both areas.
- Night‑time cough, sour taste on waking, hoarseness: reflux contributing.
Self‑care cheat sheet (print this):
- Hydration target: pale urine colour; take warm fluids every couple of hours on bad days.
- Gargle schedule: salt water after meals and before bed.
- Nasal routine: saline rinse morning and evening; steroid spray once daily if allergic or very blocked.
- Med timing: paracetamol/ibuprofen staggered per label to smooth pain/fever spikes.
- Sleep setup: side‑lying with head slightly raised; keep the room aired.
- Track it: note day 1 of symptoms, any fever, and whether things improve or worsen by day 3 and day 10.
Decision cues you can trust:
- Throat: 0-1 FeverPAIN = self‑care; 2-3 = delayed prescription; 4-5 = consider same‑day GP assessment/rapid test.
- Sinus: improving by day 10 = self‑care; no improvement or double‑worsening after initial improvement = GP review.
- Any red flag symptoms listed earlier = urgent assessment today.
Mini‑FAQ
- Can tonsillitis cause a sinus infection? Yes. Swollen tonsils make you mouth‑breathe and dry out your nasal passages, slowing sinus drainage. Germs also shuttle through the shared nasopharynx. The reverse is true: sinus drip can inflame the tonsils.
- Is this contagious? Viral and strep throat are spread by droplets and close contact. Sinusitis itself isn’t “catchy,” but the colds that trigger it are.
- Do I always need antibiotics? No. NICE data shows most sore throats and sinus infections settle without them. Antibiotics help most when FeverPAIN is 4-5 (throat) or when sinus symptoms are severe or >10 days.
- What about tonsil stones? Post‑nasal drip and repeats of throat inflammation can encourage tonsil crypt debris. Good hydration, gargles, and addressing nose issues reduce them. If stones are constant and smelly, discuss options with your GP.
- Could this be allergies, not infection? If you’re sneezy with itchy eyes and clear mucus, it’s likely allergy‑led. Steroid nasal sprays and antihistamines help. Untreated allergies often set off both throat and sinus problems.
- Do probiotics, zinc, or vitamin C work? Evidence is mixed. They won’t fix a clear bacterial infection, but they’re generally safe when used sensibly. Prioritise sleep, fluids, and nasal/throat care first.
- Why do kids get this more? Big adenoids/tonsils, small noses, and school germs. If a child snores loudly, has pauses in breathing, or struggles to eat, seek a GP/ENT referral.
- Is a deviated septum relevant? It can be. Poor airflow and drainage raise sinusitis risk. If symptoms persist despite good medical care, an ENT can assess.
- Will removing tonsils stop sinus infections? Not necessarily. It may reduce severe throat attacks. If sinus disease is the main problem, you need a nose/sinus plan; sometimes adenoids matter more in children.
Real‑world examples
- Teacher, late autumn: gets a cold, then 5 days of facial pressure and a raspy throat. FeverPAIN is 1. She uses saline rinse, fluticasone spray, paracetamol, gargles, and night‑time honey. By day 8, she’s 70% better-no antibiotics needed.
- Student, exam week: week‑long sore throat with pus and fever, no cough. FeverPAIN is 4. Rapid strep test positive; short course of penicillin clears it. He changes toothbrush and uses saline rinses to prevent another round.
- Child, age 6: springtime snoring, blocked nose, mouth breathing, morning sore throats. Allergy plan (steroid spray, antihistamine, nightly saline) reduces symptoms. ENT later finds enlarged adenoids; adenoidectomy considered after persistent glue ear.
Prevention checklist
- Allergy control in season: daily steroid spray + antihistamine as needed.
- Saline rinse after dusty days, flights, or during a cold.
- Hydrate early at the first sign of a scratchy throat.
- Smoke‑free home and car; avoid vaping clouds.
- Vaccines up to date (flu, COVID‑19) to blunt severe viral triggers.
- Replace toothbrush 24-48 hours after starting antibiotics for strep.
- Keep work/school desk clean and wash hands regularly.
When to ask for an ENT referral
- Recurrent severe sore throats meeting NHS Evidence‑Based Interventions thresholds (7 in 1 year, 5 per year for 2 years, or 3 per year for 3 years), and they’re disabling.
- Documented quinsy (peritonsillar abscess) or sleep‑disordered breathing/snoring with daytime effects.
- Chronic rhinosinusitis for 12+ weeks despite regular saline and steroid spray, or if nasal polyps are suspected.
- Children with persistent nasal blockage, recurrent ear infections, or suspected enlarged adenoids affecting sleep or feeding.
UK‑specific tips that make a difference
- Use FeverPAIN rather than Centor; it performs well in UK primary care.
- Pharmacies can advise on nasal steroids and saline options without a prescription.
- For worsening symptoms out of hours, NHS 111 can guide you to urgent care if needed.
- Keep a simple symptom diary; it helps your GP decide on antibiotics or referral faster.
Final quick reference
- Day 1-3: comfort care, saline, steroid nasal spray if congested/allergic; no rush to antibiotics.
- Day 4-7: if throat is still intense and FeverPAIN is 4-5, contact your GP. If sinus pressure persists but gradually improves, keep the plan.
- Day 8-10: if sinus symptoms are unchanged or worse, or there’s double‑worsening, see your GP about possible antibiotics.
- Any red flags at any point: seek urgent care today.
If you remember one thing: the nose and throat are teammates. Calm the nose, and the throat follows. Soothe the throat, and the nose drains. Build a simple daily routine-saline, a steroid spray when needed, pain relief, gentle gargles-and most people stop ping‑ponging between infections. If you’re still stuck after a few well‑run cycles, that’s your cue to discuss an tonsillitis or sinus game plan with your GP, and ask whether allergies, reflux, adenoids, or a structural nose issue need attention.


Comments
this post is so long i fell asleep reading it. like bruh i just have a sore throat not a phd thesis. 🤡
you know what this is really about? it's not the sinuses or the tonsils-it's the collective trauma of modern life. we're breathing polluted air, sleeping in climate-controlled tombs, and swallowing antibiotics like candy. the body is screaming for connection, not saline sprays. we're not broken-we're betrayed by the system.
FeverPAIN is solid but most docs don't even know what it is. I've had 3 rounds of amoxicillin for viral stuff because the nurse just clicked 'antibiotics' without asking. Saline rinse works better than half the prescriptions i've gotten. just sayin'
the real tragedy isn't the biofilm or the adenoids-it's that we've outsourced our immune intelligence to pharmaceutical brochures. we don't listen to our bodies anymore. we check fever scales and symptom checklists like they're horoscopes. the body remembers. it knows when to burn, when to rest, when to weep. we just forgot how to be quiet long enough to hear it.
I must respectfully submit that the structural and physiological interplay between the nasopharyngeal lymphoid ring and mucociliary clearance mechanisms is, in fact, a paradigmatic exemplar of human immunological architecture. One cannot simply dismiss the role of adenoid hypertrophy without acknowledging the intricate neuroimmunological feedback loops at play.
sooo... you're telling me my 7th sinus infection this year is because i breathe? 🙄 like maybe my body is just tired of being told to 'just use a neti pot' while my landlord refuses to fix the mold in the walls? i'm not lazy, i'm traumatized. and yes, i cried during the saline rinse. it was cathartic.
ok but have you tried quantum healing? like literally visualize your tonsils as glowing crystals and your sinuses as rainbow rivers? i did it after my 3rd round of antibiotics and now i only get sick when i'm emotionally blocked. also i drink moon water. it helps. 🌙✨
you got this!! i used to bounce between throat and nose for years but saline rinse + humidifier + just resting when i felt off changed everything. no guilt, no pressure. your body just needs a break. you're doing better than you think 💪❤️
in my village in Nigeria, we use ginger tea with honey and steam from boiled eucalyptus leaves. no sprays, no pills. just warmth and patience. i came to Canada and got lost in all these guidelines. sometimes the oldest remedies are the ones that remember your body before it became a checklist. your throat isn't a problem to fix-it's a messenger. listen.
this is so helpful!! 🙌 i printed the cheat sheet and taped it to my fridge. also i use the salt water gargle and now my partner says i smell like a beach 🏖️ lol. thank you for not making me feel dumb for asking if my tonsils are 'supposed to be this swollen'
i think the real fix is learning to breathe through your nose again. not just with sprays but with awareness. like when you're sitting at your desk, pause and feel your breath. if you're mouth breathing, gently close your lips. it sounds silly but it rewires your whole system. i did it for 3 weeks and my sinuses stopped acting up
this whole thing is a scam. big pharma and the ENT industry are pushing this 'cycle' narrative so you keep buying sprays, rinses, and eventually surgery. the real cause? 5G towers and fluoridated water. your immune system is being poisoned by the government's secret bio-weapons program. i've been researching this for 12 years. they don't want you to know the truth.
look i get it, we're all just little bacteria colonies trying to survive in a capitalist nightmare. but honestly? if you're not from the UK and you're following NICE guidelines like they're scripture, you're kinda missing the point. in america, we just take a nap, drink chicken soup, and pray to the god of insurance coverage. also, who the hell has time to gargle 4 times a day? i'm a single dad with 3 kids and a 60-hour workweek. give me a pill or leave me alone.
I must point out that the use of the term 'biofilm-forming bacteria' is scientifically accurate, yet the casual tone of this post undermines its credibility. Additionally, the omission of peer-reviewed citations for the FeverPAIN criteria-while referenced-is a glaring oversight in an otherwise meticulously structured piece. One must maintain rigor, even in informal forums.
The author's conflation of symptomatic relief with therapeutic resolution represents a fundamental epistemological failure in contemporary medical communication. The proliferation of 'self-care cheat sheets' infantilizes the patient, replacing clinical discernment with algorithmic compliance. One does not 'manage' a lymphatic system with saline and honey. One must confront the ontological dissonance between biological reality and consumerist health culture.
I'm sorry, but 'saline rinse morning and evening'? That's not a 'routine'-that's a full-time job. And why is 'honey' recommended but not 'raw, local, unpasteurized, organic honey'? And why no mention of the glycemic index impact on immune response? This is sloppy. And you missed the fact that tonsil stones are often caused by Candida overgrowth-did you even read the literature?
i read this whole thing. zero points. just give me a pill. 🤷♀️