What Is Statin Intolerance, Really?
Most people hear "statin intolerance" and think: statin side effects are too much to handle. But that’s not the full story. Statin intolerance isn’t just about feeling sore muscles after taking a pill. It’s a clinical diagnosis - one that requires a careful, step-by-step process to confirm. Too often, patients are told they’re intolerant after just one bad reaction, then told to stop statins for good. That’s dangerous. Statins cut heart attacks and strokes by 20-25% for every 1 mmol/L drop in LDL cholesterol. For millions, stopping them means trading proven protection for unproven relief.
The truth? Only 5-15% of people who say they can’t take statins actually have true statin-associated muscle symptoms (SAMS). The rest? Their symptoms might be from something else - low vitamin D, an underactive thyroid, or even a nocebo effect where expecting side effects makes them happen. That’s why structured statin intolerance clinics exist. They don’t just listen. They test. They rechallenge. They rebuild.
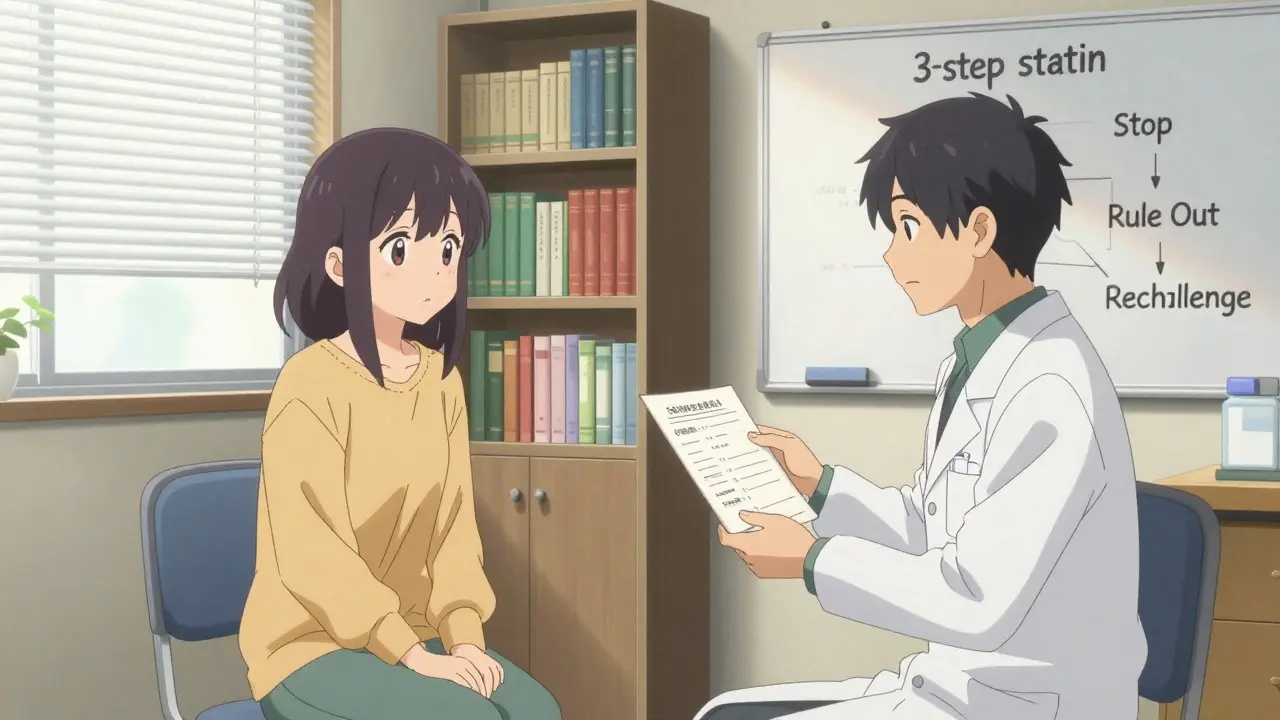
How These Clinics Work: The 3-Step Protocol
At a well-run statin intolerance clinic, you don’t just walk in and get a new prescription. You go through a proven process. Here’s how it works:
- Stop the statin - You stop your current statin completely for at least two weeks. No partial doses. No switching brands. Just a clean break.
- Rule out other causes - Your doctor checks your thyroid, vitamin D, kidney function, and drug interactions. Did you start a new supplement? Drink more alcohol? Take a new antibiotic? These can mimic statin side effects.
- Rechallenge carefully - After symptoms fade, you’re given a different statin - usually a hydrophilic one like rosuvastatin or pravastatin - at the lowest possible dose. Sometimes, it’s even given just twice a week.
This isn’t guesswork. It’s based on guidelines from the National Lipid Association and the American College of Cardiology. Cleveland Clinic’s data shows that 72% of patients who switch to a hydrophilic statin can tolerate it. That’s more than 7 out of 10 people who were told they couldn’t take statins at all.
Why Switching Statins Makes a Difference
Not all statins are the same. Lipophilic statins - like simvastatin and atorvastatin - easily slip into muscle tissue, which is why they’re more likely to cause muscle pain. Hydrophilic statins - like rosuvastatin and pravastatin - are designed to be pulled mainly into the liver, where they do their job. They barely touch muscle.
One patient from Kaiser Permanente’s program, a 62-year-old man with a history of heart disease, was told he was statin intolerant after simvastatin gave him leg cramps. He stopped all statins for five years. At the lipid clinic, he was switched to rosuvastatin 5 mg twice a week. His LDL dropped from 142 to 89. No pain. No muscle weakness. He’s now back on a statin - just not the one he was on before.
Switching isn’t just about picking a different pill. It’s about matching the drug’s chemistry to your body’s tolerance. That’s why blanket advice like "just try a lower dose" doesn’t work. You need the right statin, at the right time, in the right way.
Intermittent Dosing: A Game Changer for the Intolerant
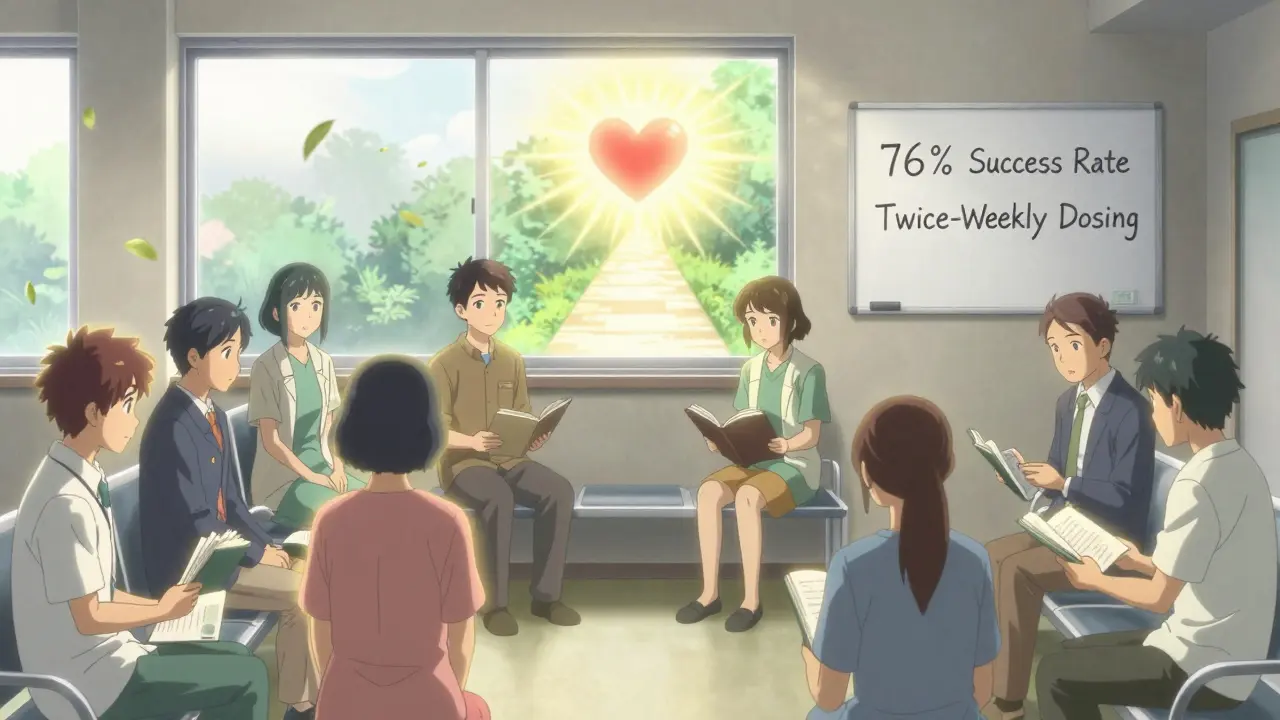
What if you can’t tolerate statins daily? There’s a solution: intermittent dosing. Instead of taking a statin every day, you take it every other day - or even twice a week. This works best with long-acting statins like rosuvastatin or atorvastatin.
A 2021 Cleveland Clinic study followed 1,247 patients who had been labeled statin intolerant. After switching to rosuvastatin 5-10 mg twice weekly, 76% were able to stay on therapy without side effects. Their LDL still dropped by 20-40%. That’s nearly as effective as daily dosing, with far fewer problems.
And it’s not just theoretical. In the UK, NHS lipid clinics are starting to use this approach routinely. Patients who can’t take statins daily often end up on this schedule. It’s cheaper than PCSK9 inhibitors. It’s safer than doing nothing. And it works.
What If You Still Can’t Tolerate Statins?
Some patients - about 5-10% - still can’t take any form of statin, even intermittently. That’s where non-statin options come in. And they’re not just expensive last resorts.
Ezetimibe is the first-line choice. It costs about $35 a month, reduces LDL by 15-20%, and cuts heart events by 6% - proven in the IMPROVE-IT trial. It’s safe, well-tolerated, and doesn’t cause muscle pain.
Bempedoic acid (Nexletol) is newer. Approved in 2020, it lowers LDL by 18% without affecting muscle tissue. It’s taken once daily and was tested in over 14,000 people in the CLEAR Outcomes trial. No increase in muscle symptoms. It costs more - around $491 a month - but many insurers cover it if you’ve tried and failed statins.
And then there are PCSK9 inhibitors like evolocumab. They’re injectables that slash LDL by 60% or more. But they cost about $5,850 a year. Insurance often denies them unless you’ve failed at least two other options. Some patients spend months appealing. But for those at high risk - like people with familial hypercholesterolemia or prior heart attacks - they can be life-saving.
What Clinics Don’t Tell You (But You Need to Know)
There’s a dark side to statin intolerance clinics. They’re hard to get into. Wait times for specialist appointments in the U.S. and UK average 6-8 weeks. In rural areas, it can be months. And not all clinics are created equal. Some still skip the rechallenge step. Others don’t check vitamin D or thyroid levels. That’s why you need to ask the right questions.
Ask: "Will you rule out other causes before calling me intolerant?" Ask: "Will you try a hydrophilic statin at a low dose?" Ask: "Will you consider twice-weekly dosing?" If the answer is no, you’re not getting the full protocol. You’re getting a quick dismissal - and that’s not good enough.
Also, don’t assume your doctor knows the latest data. A 2023 ACC survey found that only 42% of community hospitals have formal statin intolerance protocols. Academic centers? 87%. If you’re not near a big hospital, you may need to advocate harder.
Real Patients, Real Results
On Reddit, a user named HeartPatient87 wrote: "After being labeled statin intolerant for five years, the lipid clinic at Johns Hopkins had me on rosuvastatin 5mg twice weekly with CoQ10 - LDL dropped from 142 to 89 without muscle pain." That’s not a miracle. That’s protocol.
Kaiser Permanente’s internal survey found 82% of patients in their statin intolerance program were able to restart lipid-lowering therapy. Compare that to 45% in regular care. That’s a 37-point gap. That’s thousands of people who didn’t have to live with untreated high cholesterol.
One woman in Birmingham, after being told she couldn’t take statins for six years, finally got help at a local NHS lipid clinic. She was switched to pravastatin 10 mg every other day. Her LDL fell from 168 to 92. Her muscle pain vanished. She started walking again. She didn’t need a new drug. She just needed the right approach.
What’s Next? Genetic Testing and New Formulations
The future is getting smarter. Mayo Clinic started testing for the SLCO1B1 gene variant in 2023. People with this variant are more likely to get muscle pain from simvastatin. If you have it, you avoid that drug - and save yourself years of trial and error.
There’s also nanoparticle statins in phase 2 trials. These tiny particles deliver the drug straight to the liver, bypassing muscle tissue. Early results show 92% tolerability. That’s huge.
And bempedoic acid? It’s gaining ground. The FDA approved it for people with statin intolerance. The European Society of Cardiology now recommends it as a first-line alternative. It’s not perfect - it can raise uric acid levels - but for many, it’s the best option left.
What You Can Do Today
If you’ve been told you’re statin intolerant:
- Don’t accept it as final.
- Ask for a referral to a lipid specialist or statin intolerance clinic.
- Request a rechallenge with a hydrophilic statin - rosuvastatin or pravastatin - at low dose.
- Ask about twice-weekly dosing.
- Get your vitamin D, thyroid, and CK levels checked.
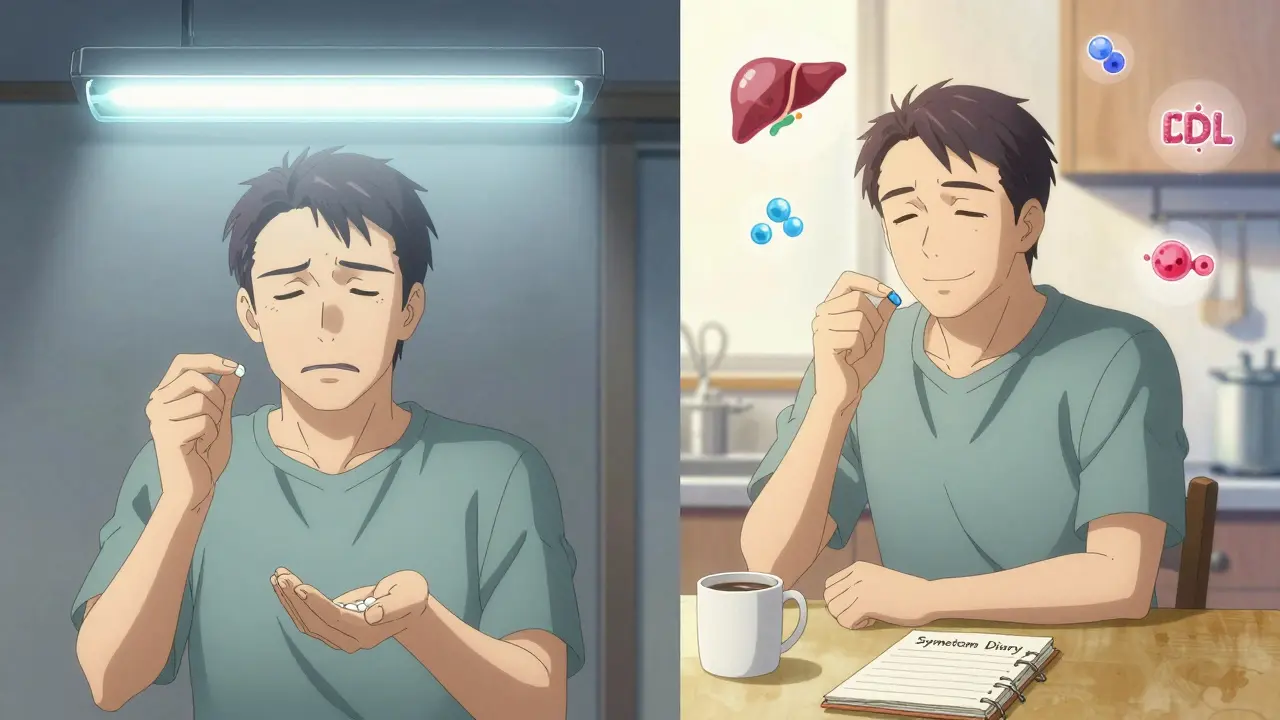
- Keep a symptom diary: when pain started, where it is, how bad it is (0-10 scale), and if it goes away after stopping the pill.
Statins save lives. But only if you can take them. Structured protocols exist to make that possible. You don’t have to choose between heart health and muscle pain. You just need the right system to help you find the middle ground.
Can statin intolerance be reversed?
Yes, in most cases. Up to 70-80% of patients labeled statin intolerant can tolerate a different statin, a lower dose, or an intermittent dosing schedule when evaluated through a structured clinic protocol. The key is proper rechallenge - stopping the statin, ruling out other causes, and trying again with a different approach. Many patients who thought they couldn’t take statins at all are successfully back on therapy.
What’s the difference between statin side effects and statin intolerance?
Statin side effects are common and often mild - like occasional muscle soreness. Statin intolerance is a clinical diagnosis: you’ve tried at least two statins, one at the lowest dose, and still had symptoms that disappeared when you stopped. It’s not about one bad reaction. It’s about consistent, reproducible symptoms that prevent you from staying on therapy. True intolerance is rare. Most people who think they’re intolerant aren’t.
Do I need a blood test to prove statin intolerance?
Not always. While CK (creatine kinase) levels above 10 times the upper limit can indicate muscle damage, many people with true statin intolerance have normal CK levels. The diagnosis is based on symptoms - muscle pain in large muscle groups (thighs, shoulders, back) that start 2-4 weeks after starting the statin and go away 2-4 weeks after stopping. Blood tests help rule out other causes, but symptoms matter more than numbers.
Is ezetimibe as good as a statin?
It’s not as strong, but it’s proven. Ezetimibe lowers LDL by about 15-20%, compared to 30-50% for statins. But in the IMPROVE-IT trial, adding ezetimibe to a statin reduced heart attacks and strokes by 6%. For people who can’t take statins, ezetimibe alone still cuts cardiovascular risk - and it’s safe, cheap, and well-tolerated. It’s the best non-statin first step.
Why do some doctors say statin intolerance is overdiagnosed?
Because studies show up to 80% of patients who report statin side effects don’t have them when tested under blinded conditions. In one trial, patients thought they had muscle pain on statins - but when given a placebo without knowing it, they still reported pain. That’s the nocebo effect. Many doctors now believe patients are told statins cause pain, so they notice normal aches and blame the pill. Structured clinics help separate real intolerance from misattribution.

Comments
I was told I was statin intolerant for years until I found a lipid clinic. Now I'm on rosuvastatin twice a week and my LDL is down to 85. No muscle pain. No drama. Just results. Why do so many docs skip this step?
People are just lazy and want to blame a pill for their own poor lifestyle. If you don't eat right and sit on your butt all day no statin in the world will save you. Stop pretending you're sick when you're just unmotivated.
I had muscle pain for months after starting atorvastatin. My doctor said 'just tough it out' so I stopped. Two years later I went to a lipid clinic and they put me on pravastatin 10mg every other day. My pain vanished. My cholesterol dropped. I wish I'd known this sooner. Seriously, if you think you're intolerant, don't give up. Find someone who knows what they're doing.
The nocebo effect is real. I had a friend who swore statins wrecked his legs. He stopped them, felt better, then got put on placebo in a trial and still complained of pain. He was convinced it was the drug. It wasn't. It was his fear. That's why structured clinics are so important. They cut through the noise.
I can't believe people still think this is just about muscle pain. It's not. It's about control. Doctors don't want to spend an hour with you. They want to write a script and move on. But if you're one of the 80% who were misdiagnosed? You're left with untreated cholesterol. And that's a death sentence waiting to happen. Don't let them dismiss you. Fight for your life.
I just want to say, if you're reading this and you've been told you're statin intolerant, please, please, please don't accept that as your final answer. There are so many options: hydrophilic statins, intermittent dosing, ezetimibe, bempedoic acid. And yes, even PCSK9 inhibitors if you qualify. Your heart deserves a fighting chance. Ask for a referral. Ask for testing. Ask for a second opinion. You are not alone. And you are not powerless.
My mom was told she couldn't take statins for 7 years. She had heart disease. She was scared. Then she went to a clinic in Denver. They did the full protocol. Switched her to rosuvastatin 5mg twice a week. Her LDL went from 156 to 88. She started gardening again. She didn't need a miracle. She just needed someone who knew how to listen.
statins are just big pharma's way to make money. they dont really work. the body knows how to balance itself. you dont need pills. you need to meditate and eat raw food. my cousin in delhi took turmeric and his cholesterol dropped. why do you trust a pill more than nature?
I used to think this was all hype. Then my brother got referred to a lipid clinic after being told he was intolerant for 4 years. He’s now on twice-weekly rosuvastatin and feels better than he has in a decade. It’s not magic. It’s science. And it’s accessible if you know where to look.
This is exactly why we need more lipid specialists. Not just in cities. In rural clinics too. My cousin in Nebraska waited 11 weeks for an appointment. By then, his LDL was 210. He had a mild heart attack. If they'd had a protocol in place, he'd have been on ezetimibe or intermittent statins months earlier. We're failing people because we're too slow.
Let’s be brutally honest. The entire statin intolerance narrative is a perfect storm of medical negligence, patient misattribution, and pharmaceutical marketing. The real issue isn’t that people can’t tolerate statins-it’s that doctors don’t know how to properly diagnose or manage them. They skip the rechallenge. They don’t check vitamin D. They don’t consider hydrophilic alternatives. And then they blame the patient for not taking their pills. Meanwhile, the real problem is systemic incompetence disguised as patient care. The data is clear: 80% of these cases are misdiagnosed. That’s not a flaw in the drug. That’s a flaw in the system. And until we fix that, people will keep dying unnecessarily.
I cried when I finally got on twice-weekly rosuvastatin. After six years of thinking I was broken, I realized I just needed the right key. Not more pills. Not more guilt. Just the right one. Now I hike every weekend. My legs don’t ache. My heart is safer. And I’m not just surviving-I’m living. This isn’t about drugs. It’s about being seen.