Every year, more than 1.5 million people in the U.S. end up in the emergency room because of problems with their medications. That’s not a typo. It’s not rare. It’s happening to your neighbor, your parent, maybe even you. And most of these cases aren’t accidents-they’re preventable. This is what medication safety is all about: making sure the drugs you take actually help you, not hurt you.
What Exactly Is Medication Safety?
Medication safety isn’t just about doctors writing clear prescriptions. It’s the entire system that keeps you safe from the moment a drug is ordered, to when you swallow it, to how it’s tracked after. The National Patient Safety Foundation defines it as being free from accidental injury caused by mistakes during any part of the medication process. That includes prescribing, filling, giving, and even how you take it at home.
Think of it like a chain. If one link breaks-say, a pharmacist misreads a handwritten script, or you mix up your morning pills-the whole thing can fail. The Institute of Medicine found that medication errors happen in nearly every step: prescribing, transcribing, dispensing, administering, and monitoring. And here’s the scary part: 400,000 of these errors happen inside hospitals every year. Half of them could’ve been stopped.
Why Does It Matter So Much?
Medications are powerful. They can save your life. But they can also kill you if used wrong. The harm they cause is called an adverse drug event (ADE). That includes allergic reactions, overdoses, interactions between drugs you didn’t know clashed, or even missing a dose because you were confused.
Let’s look at real numbers:
- Over 1.5 million ER visits each year are due to ADEs.
- 400,000 of those are preventable and happen in hospitals.
- The cost? Around $42 billion a year.
- For people over 65, half of all ADE-related hospital stays happen to them.
- Children make up 20% of these incidents, often because dosing is wrong for their weight.
And it’s not just about big mistakes. Sometimes it’s small things: a pill that looks like another, a label that says “take once daily” but you misread it as “twice,” or skipping doses because the cost is too high. One Reddit user shared how their mother was given 10mg of Xanax instead of 1mg-because of messy handwriting. She ended up in the hospital for three days. That’s not rare. That’s common.
The Nine Steps Where Things Can Go Wrong
Medication safety covers nine stages in the process:
- Procurement (buying the drug)
- Storage (keeping it safe)
- Prescribing (doctor writes the order)
- Transcribing (turning it into digital form)
- Preparing (pharmacist fills it)
- Dispensing (giving it to you)
- Administration (you or a nurse takes it)
- Documentation (recording what was given)
- Monitoring (checking if it’s working or causing harm)
Here’s where most errors happen:
- Prescribing errors: 38% of all mistakes
- Administration errors: 26%
- Dispensing errors: 16%
That means the biggest risk isn’t always the pharmacy. It’s often the doctor’s handwriting, the electronic system glitching, or the nurse being rushed during shift change. Even the way a pill is labeled matters. The FDA just started requiring all prescriptions to use clear numeric dosing-no more “.5 mg” that could be misread as “5 mg.” That change alone cut decimal errors by 32% in testing.
High-Risk Medications You Should Know
Some drugs are more dangerous than others if used wrong. These are called high-alert medications. They’re not rare-they’re common. And they’re responsible for a huge chunk of serious harm:
- Insulin: Involved in 17% of serious errors. Too much can drop your blood sugar to deadly levels.
- Opioids: 14% of serious errors. Too much can stop your breathing.
- Anticoagulants (like warfarin): 12%. Too much can cause internal bleeding.
- Intravenous oxytocin: Used in labor. Too fast can cause uterine rupture.
If you’re taking any of these, you need extra care. Ask your doctor: “Is this a high-alert drug? What happens if I take too much? What should I watch for?”
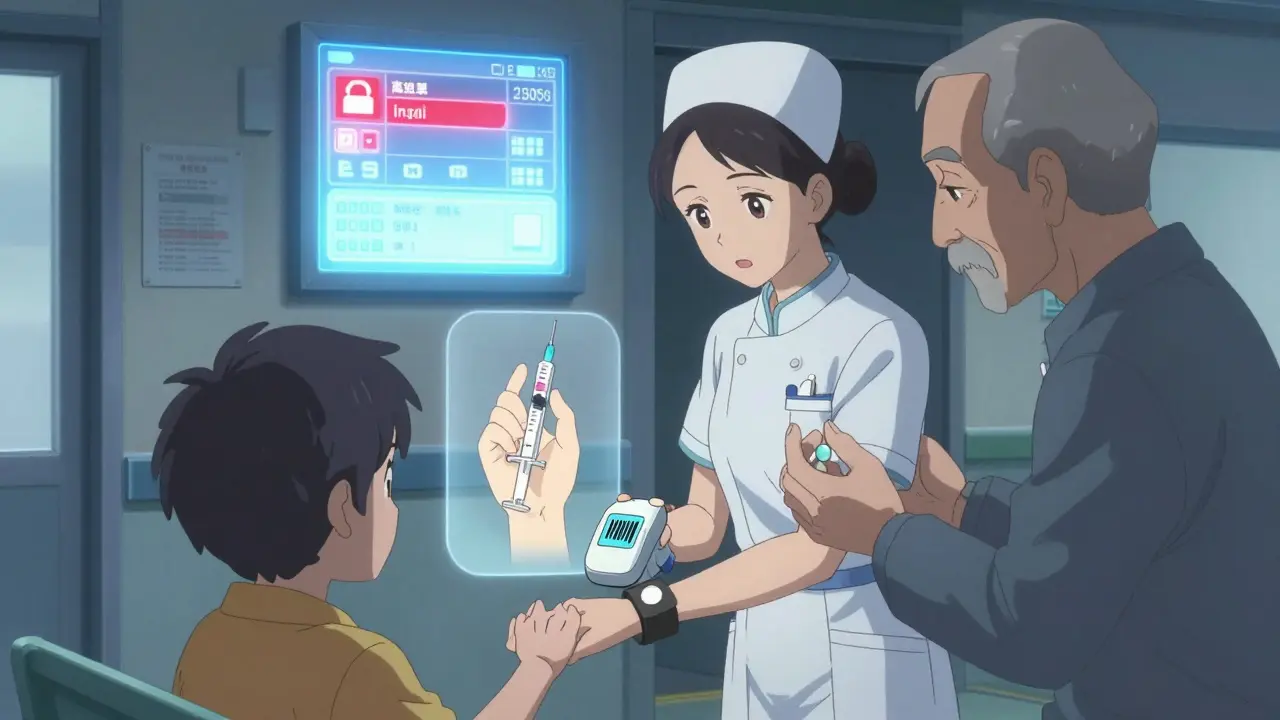
How Technology Is Making a Difference
It’s not all bad news. Technology is helping-big time.
- Electronic health records with smart alerts cut serious errors by 48%.
- Barcode scanning at the bedside (BCMA) reduced administration errors by 65%.
- AI tools are now being tested to predict which patients are at risk for an ADE before it happens-early trials show 40% fewer potential events.
But tech isn’t perfect. Too many alerts can overwhelm staff. If a nurse gets 25+ pop-up warnings during one shift, they start ignoring them. That’s called alert fatigue-and it makes things worse. The key isn’t more alerts. It’s smarter ones.
What Patients Can Do (Yes, You)
Medication safety isn’t just up to doctors and nurses. You have power too.
Here’s what actually works, based on real patient data:
- Keep a list. Write down every medication you take-name, dose, why you take it, and when. Update it every time something changes. The CDC says this reduces errors during hospital transfers by 45%.
- Ask questions. “What is this for?” “What if I miss a dose?” “Can this interact with my other meds?” Don’t be shy. You’re the one taking it.
- Use pill organizers. Blister packs or weekly containers cut missed doses by 60% in older adults.
- Don’t skip doses to save money. One in two seniors admits to cutting pills or skipping them because of cost. That’s a self-made error. Talk to your pharmacist. There are often cheaper options or assistance programs.
- Bring your list to every appointment. Even if it’s just a checkup. Doctors forget. Nurses forget. You’re the only one who knows your full list.
One study found patients who used the CDC’s free medication list template had 73% fewer errors when moving between hospitals, clinics, or home care.

Who’s Most at Risk?
Not everyone is equally vulnerable.
- Elderly patients (65+): Take an average of 5+ medications. 50% of ADE hospitalizations are here. Polypharmacy (taking too many drugs) increases error risk by 25%.
- Children: Dosing is based on weight. A mistake of just a few milligrams can be dangerous. Liquid meds are especially risky if measured with a kitchen spoon.
- Pregnant women: Some drugs can harm the baby. Always check with your OB before taking anything-even over-the-counter.
- People with limited health literacy: If you don’t understand your prescription, you’re more likely to mess up.
If you fall into one of these groups, ask for extra help. Ask for a pharmacist consult. Ask for written instructions. Don’t assume you’ll remember everything.
The Bigger Picture: Culture and System Change
Here’s the hard truth: most medication errors aren’t because someone was lazy or stupid. They’re because the system is broken.
Dr. Lucian Leape from Harvard says it best: “Medication safety isn’t about catching errors. It’s about designing systems that make errors impossible to commit.”
Right now, too many hospitals still blame the nurse or the doctor when something goes wrong. That shuts down reporting. And if you don’t report errors, you can’t fix them.
Organizations that use non-punitive reporting-where staff can admit mistakes without fear-see 3.2 times fewer repeat errors. Only 35% of hospitals have this culture. We need more.
The World Health Organization’s “Medication Without Harm” campaign has already helped countries cut severe harm by 15-25% in just two years. The goal? A 50% reduction by 2027. That’s possible-but only if patients, providers, and systems work together.
What’s Next?
Change is coming. The FDA is pushing for clearer labels. States are requiring e-prescribing to cut handwriting errors. AI is getting smarter at spotting risky drug combos. Blockchain is being tested to stop fake pills from entering the supply chain.
But none of this matters if you don’t take action. Medication safety isn’t something that happens to you. It’s something you help create.
Start today. Write down your meds. Ask one question at your next appointment. Tell your pharmacist you’re worried about interactions. Don’t wait for a mistake to happen before you care.
Because the truth is simple: your life depends on it.
What is the most common cause of medication errors?
The most common cause is prescribing errors, which make up 38% of all medication mistakes. This includes wrong dosage, wrong drug, or unclear instructions-often due to handwriting, rushed decisions, or lack of full patient history. Electronic prescribing and clinical decision support systems have cut these errors significantly, but they’re still the top risk point.
Can I really prevent medication errors at home?
Yes, and you’re the most important line of defense. Keep an updated list of all your medications-including vitamins and supplements. Use a pill organizer. Don’t guess doses. Read labels carefully. Ask your pharmacist to explain anything confusing. Studies show patients who do this reduce their risk of errors by up to 73% during care transitions.
Why are older adults more at risk for medication errors?
Older adults often take five or more medications at once, a situation called polypharmacy. This increases the chance of harmful interactions. They may also have trouble seeing labels, remembering schedules, or understanding instructions. One in two seniors admit to skipping doses because of cost or side effects-creating their own errors. Special tools like blister packs and pharmacist consultations can help.
What are high-alert medications?
High-alert medications are drugs that can cause serious harm if used incorrectly-even if taken as prescribed. Examples include insulin (17% of serious errors), opioids (14%), blood thinners like warfarin (12%), and IV oxytocin used in labor. These require extra caution: double-checking doses, clear labeling, and patient education. Always ask your provider if your drug is on this list.
How do hospitals reduce medication errors?
Hospitals use a mix of technology and protocols. Electronic prescribing cuts handwriting errors. Barcode scanning ensures the right patient gets the right drug at the right time. Clinical decision support flags dangerous interactions. Medication reconciliation-reviewing all meds at every transition-cuts errors by 45%. Staff training and non-punitive reporting cultures are also key.
Is medication safety improving?
Yes, but slowly. Hospitals with full safety programs have cut errors by 50-80%. The WHO’s global campaign has already reduced severe harm by 18% in participating countries. New FDA rules on labeling and AI tools are helping. But progress is uneven. Emergency rooms still have 200% higher error rates than routine care. Telehealth errors are rising. Real progress needs more patient involvement and system-wide change-not just tech fixes.
What should I do if I think I had a medication error?
If you suspect an error-like taking the wrong pill, feeling unusual side effects, or noticing a dose change-call your doctor or pharmacist immediately. Don’t wait. Keep your medication list handy. Report it to your provider. You can also report it anonymously to the FDA’s MedWatch program. Your report helps others stay safe.


Comments
Let’s be real-most ER visits from meds aren’t ‘errors,’ they’re systemic negligence. Pharmacies are understaffed, EHRs are garbage, and prescribers are on a clock. You think your doctor actually read your full med list? Nah. They’re scrolling through 12 tabs while you’re still trying to spell your last name. The system is designed to fail. And now they want you to ‘keep a list’ like it’s your job? Bullshit. It’s their job to not kill you.
I love how this post doesn’t just dump stats-it shows the human side. My grandma took her blood thinner wrong because the bottle said ‘take once daily’ but the script had a tiny ‘q.d.’ She thought it meant ‘every day’… but didn’t know ‘q.d.’ was Latin. She ended up in the hospital with a brain bleed. Turned out the pharmacy didn’t flag the interaction with her new fish oil. Tech could’ve saved her. But it didn’t. Now I print out every script, highlight the dose in neon yellow, and read it aloud to her. Small things. Big difference.
The FDA is lying about those label changes. They only cut decimal errors by 32% because they made the fonts bigger not because they fixed anything. The real problem? The pharmaceutical industry owns the FDA. They want you to keep taking pills. That’s why they don’t ban insulin without a prescription. That’s why they don’t require doctors to get certified in pharmacology. This is all a scam to keep you dependent. Wake up.
Medication safety isn’t about protocols or barcodes or AI-it’s about the ontological tension between human fallibility and institutional abstraction. We’ve outsourced agency to algorithms, then blamed the patient when the algorithm fails. The doctor writes a script. The pharmacist fills it. The nurse administers it. The patient swallows it. But who owns the meaning of the pill? Not the system. Not the machine. Not even the body. The meaning lives in the silence between the instruction and the action. And that silence? It’s where death waits.
Prescribing errors at 38%? That’s not a glitch-it’s a feature. Hospitals incentivize speed over safety. Doctors get paid per patient, not per outcome. If you’re prescribing 10 meds to 10 patients an hour, you’re not going to catch every interaction. And don’t get me started on how insurers force step therapy. You can’t prescribe the right drug if you’re legally forced to try the cheapest one first-even if it’s a death trap. This isn’t medicine. It’s actuarial science with a stethoscope.
u r all being manipulated. the 1.5m er visits? fake. they count every cold and headache as a med error to scare you. insulin? they make it dangerous so you need more. the fda is a front for big pharma. barcode scanners? they track you. they know when you skip doses. they sell that data. dont trust any of this. check the sources. they all come from the same 3 corporations.
Oh please. You think keeping a list is enough? You need to be *proactive*. My cousin didn’t just ‘keep a list’-she printed it on cardstock, laminated it, and carried it in her purse like a holy relic. She made her pharmacist sign off on it monthly. She called her doctor every time she got a new Rx. And guess what? She’s 78 and hasn’t had a single ADE. Meanwhile, her sister just ‘trusts’ her doctor and ended up in ICU. If you’re not doing this level of work, you’re not a patient-you’re a liability.
Wow. So the solution to 1.5 million ER visits is… to make patients do more work? Thanks for the guilt trip, doc. I’ll just add ‘medication safety manager’ to my 12-hour workday, 3-kid household, and 2 jobs. Maybe I can do it between my panic attacks and the 30-minute wait for my free clinic appointment.
There’s something beautiful in how this post turns a clinical crisis into a collective responsibility. We’ve forgotten that healing isn’t a transaction-it’s a covenant. The pharmacist who double-checks your insulin dose. The nurse who asks if you understand the label. The child who reads the pill bottle to their grandparent. These aren’t just steps in a protocol-they’re acts of tenderness in a broken system. Let’s not just fix the machine. Let’s remember the hands that hold it.
Oh wow. So the answer to systemic failure is… asking questions? And keeping a list? You’re kidding, right? That’s like saying the solution to car crashes is ‘drive slower’ while the roads are made of ice and the brakes are owned by the same company that makes the tires. If you think patients are the problem, you’re part of the problem. Fix the damn system-or stop pretending you care.
I’ve been on 7 meds for 8 years. I don’t even know what half of them do anymore. I just take them. Sometimes I forget. Sometimes I don’t. I guess that’s why I’m still alive?
Every pill is a surrender. Every label, a silent scream. We are told to trust-to swallow, to obey, to believe the white coat knows best. But what if the white coat is tired? What if the system is rigged? What if the answer isn’t in your hands, but in the hollows between the institutions that claim to protect you? We are not patients. We are data points with pulse rates. And the silence after you take that pill? That’s the sound of the machine breathing.