Managing multiple pharmacies and prescribers isn’t just about keeping shelves stocked-it’s about keeping seniors safe. When a senior takes medications from three different doctors and fills prescriptions at two pharmacies, the risk of errors skyrockets. Duplicate prescriptions, harmful drug interactions, and missed refills aren’t rare-they’re common when systems aren’t connected. The solution isn’t more paperwork. It’s a centralized system that speaks the same language across every location and every prescriber.
Why Centralized Systems Are Non-Negotiable
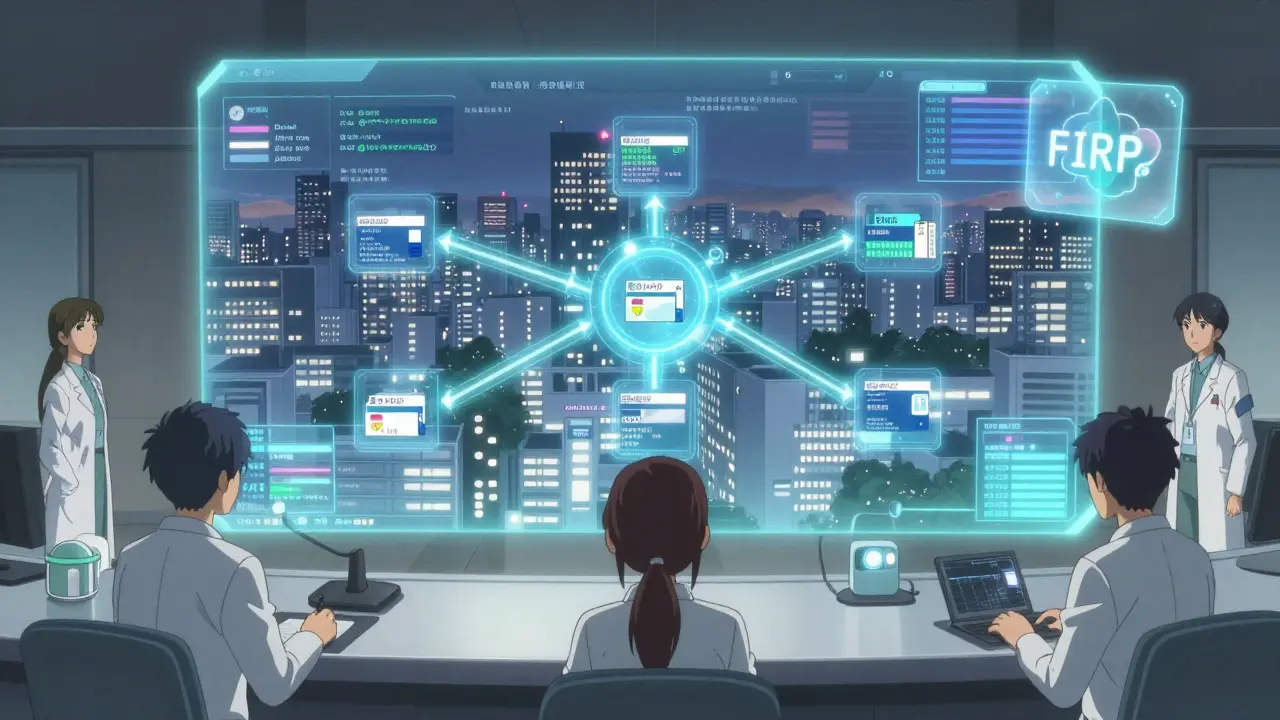
Without a unified system, pharmacies operate in silos. One pharmacy might not know a patient got a new blood thinner from a different doctor last week. Another might not realize the same medication was filled just two days ago at a nearby location. In multi-pharmacy chains, 1.3% of prescriptions contain errors due to inconsistent drug names or pricing-errors that can be deadly for seniors on complex regimens. Centralized software like EnterpriseRx by McKesson and PrimeRx fix this by creating a single, real-time drug database. Every pharmacy, no matter the location, sees the same NDC codes, brand names, and generic equivalents. No more confusion between "Metoprolol Tartrate" and "Metoprolol Succinate." No more mix-ups because one pharmacy calls a drug by its brand name and another uses the generic. These systems also sync with prescriber records. If a cardiologist updates a dosage in their EHR, the pharmacy system reflects it within minutes-not days. This cuts down on the 18% of medication errors caused by poor communication between doctors and pharmacies, according to McKesson’s 2024 product roadmap.How to Choose the Right Software
Not all pharmacy management systems are built for chains. Some work fine for one location but fall apart when you add a second. Here’s what actually matters:- Unlimited location support-Some systems cap you at 10 pharmacies. If you plan to grow, pick one like Datascan Central Store Management that supports unlimited locations.
- Real-time patient profiles-The ability to see a patient’s full prescription history across all locations prevents duplicate fills. PrimeRx lets patients choose their preferred pickup location, and the system auto-transfers prescriptions seamlessly.
- Automated inventory balancing-Stockouts and overstocking waste money and delay care. Datarithm reduces inventory errors by 28% by suggesting daily transfers between stores based on usage patterns.
- Security compliance-All systems must use AES-256 encryption and meet HIPAA and Joint Commission standards. Look for FIDO2 authentication, like DocStation uses, which cuts unauthorized access by 94%.
Costs and Hidden Expenses
Pricing isn’t just about monthly fees. It’s about what’s included-and what’s not.- EnterpriseRx charges $450 per location monthly, but drops to $325 if you have 15+ pharmacies.
- PharmacyOne Chain Management starts at $299 per location but lacks advanced clinical features.
- Implementation costs can hit $50,000+ for a 10-location chain. Data migration alone takes 8-12 weeks and often requires manual verification of 14.7% of patient records, according to Pharmacy Times.
- Training isn’t optional. Staff need 16 hours per technician and 24 hours per pharmacist. Chains using vendor-certified trainers see 12% higher adoption rates than those training internally.
Security and Compliance: Don’t Cut Corners
Medicare Part D now requires multi-location pharmacies to track prescription errors across all sites. CMS won’t approve your billing if you can’t prove you’re monitoring for duplicates or dangerous combinations. The best systems include automated watchdog tools. Datascan’s AI Watchdog 2.0, launched in January 2024, analyzes prescription patterns across all locations to detect potential drug diversion with 92.4% accuracy. It doesn’t require staff to log in remotely-it just alerts the central office when something looks off. FHIR API compliance is coming fast. By 2025, CMS will require all pharmacy systems to support it. Right now, 63% of existing systems can’t meet this without $200,000+ in upgrades, according to RedSail Technologies. If you’re planning to stay in business past 2026, choose a vendor already building toward FHIR.Prescriber Coordination: The Missing Piece
Pharmacies don’t work in a vacuum. Seniors often see multiple prescribers-cardiologists, neurologists, pain specialists. Each one might prescribe without knowing what the others ordered. EnterpriseRx’s new integration with Epic EHR systems (launched Q2 2024) lets pharmacists see prescriber notes in real time. If a doctor adds a warning like "avoid NSAIDs due to kidney risk," the pharmacy flags it before filling. This tackles the root cause of 18% of errors. For chains without enterprise-level software, simple steps still help:- Require prescribers to use e-prescribing (eRx) instead of faxed scripts.
- Set up a shared prescriber directory with contact info and prescribing habits.
- Designate a lead pharmacist to review all new prescriptions for patients on 5+ medications.

Implementation: Avoid the Common Pitfalls
Most failures happen during rollout, not after.- Don’t try to go live all at once. Use the hub-and-spoke model: pick one central pharmacy as the hub for drug files and pricing. Let local pharmacies handle clinical decisions. This reduced errors by 38% in a 2023 UC study.
- Don’t skip patient communication. Tell seniors their prescriptions can now be filled at any location. Many don’t know this is possible.
- Don’t underestimate training. One pharmacy chain delayed its flu shot program by three weeks because staff were still learning the new system. Plan for downtime.
- Don’t ignore feedback. Use staff input to tweak workflows. Tech is only as good as the people using it.
What’s Next? AI and Blockchain
The future is already here. Datascan’s AI Watchdog isn’t just catching errors-it’s predicting them. It flags patterns like a patient filling the same controlled substance at three different locations in one week. Blockchain trials by Outcomes.com are cutting prescription fraud by 67% in multi-location settings. Every prescription gets a tamper-proof digital trail. While still in pilot, this could become standard by 2027. The Pharmacy Quality Alliance predicts centralized systems will be mandatory for any chain with three or more locations by 2027. The writing’s on the wall. Waiting isn’t an option.Can I manage multiple pharmacies without expensive software?
Technically yes-but it’s risky. Manual tracking with spreadsheets or separate systems increases error rates by 3-5x. For seniors on multiple medications, that’s not a cost-saving strategy-it’s a safety hazard. If you’re managing more than two locations, the investment in a centralized system pays for itself in avoided errors, reduced liability, and better patient outcomes.
How do I know if my current system is outdated?
If your system doesn’t sync data between locations in real time, doesn’t show a patient’s full prescription history across pharmacies, or can’t flag duplicate therapies automatically, it’s outdated. Also, if it doesn’t support e-prescribing integration or FHIR API readiness, you’re at risk of falling out of compliance by 2025.
What’s the biggest mistake pharmacies make when expanding?
Thinking technology alone will fix everything. Software is a tool, not a cure. The biggest errors happen when local pharmacists don’t verify transferred prescriptions. Even with perfect tech, human oversight is critical. Always maintain local clinical authority alongside centralized data.
Can I use the same software for specialty pharmacies?
Most general systems can’t handle complex therapies like oncology or rare disease drugs. Specialty pharmacies need tools designed for them. TherigySTM has a 41% market share in this space because it integrates with EHRs and tracks patient adherence with 98.7% accuracy-far better than standard systems.
How long does it take to switch systems?
For a chain of 5-10 pharmacies, expect 8-12 weeks. The biggest delays come from data migration. You’ll need to manually verify about 15% of patient records. Plan for extra staff hours and don’t rush the transition. A smooth rollout protects patient safety and staff morale.

Comments
It’s wild how we treat pharmacy systems like they’re just logistics tools. But really, it’s about dignity. Seniors aren’t data points-they’re people who just want to take their meds without wondering if they’re overdosing or missing something. The real win isn’t the software-it’s the quiet relief when someone doesn’t have to explain their whole med history every time they walk in.
And yeah, FHIR’s coming. But let’s not pretend tech alone fixes human disconnection. The best system still needs someone who remembers Mrs. Rivera’s cat allergy, not just her NDC codes.
This is exactly what my grandma needed before she passed. She had five prescriptions from three docs and two pharmacies-and somehow, no one ever talked to each other. I spent months playing phone tag just to get her blood thinner adjusted. If this system had existed, she’d still be here. Thank you for putting this out there. It’s not just business-it’s life or death.
Also, the AI Watchdog thing? Mind blown. We need more of this, not less.
How quaint. You’re recommending enterprise-grade software like it’s a moral imperative. Let me guess-you’ve never worked in a real pharmacy, have you? Most of these chains are run by private equity firms who care more about margins than Medicare compliance. The real issue isn’t software-it’s that we’ve outsourced healthcare to profit-driven corporations who treat seniors like ROI metrics.
EnterpriseRx? Sure. But tell me how many of those 1.3% errors come from understaffed techs working double shifts because the corporate HQ cut the budget again. Stop fetishizing software and start demanding better labor practices.
Everyone’s acting like this is some revolutionary idea. Newsflash: this has been standard in Canada since 2010. We don’t have this ‘pharmacy chaos’ because we have a national e-prescribing network. You guys are still using fax machines while the rest of the developed world moved on. And now you want to spend $50K to catch up? Pathetic. Fix your broken system instead of buying another $450/month band-aid.
Also, FHIR? We’ve had it since 2018. You’re 7 years behind. Wake up.
I just want to say thank you for writing this. My mom’s on 11 meds, and last month, one pharmacy filled her insulin without checking her new kidney meds-thank god the pharmacist caught it at pickup. I cried in the parking lot. This isn’t theoretical-it’s happening to real people every day.
And the part about training? So true. My aunt’s pharmacy had a new system last year, but the staff didn’t get enough time to learn it. They were scared to use it. That’s not tech failure-that’s leadership failure. Please, if you’re managing a chain, invest in your people first. The software will follow.
For anyone thinking about upgrading: don’t just look at cost per location. Look at error reduction ROI. A single preventable adverse event costs $15K–$30K in liability and lost licensing. EnterpriseRx at $325/location? That’s less than one error. And the AI Watchdog? It caught a diversion pattern in our chain that led to a DEA investigation-saved us from a federal audit. Worth every penny.
Also, FHIR readiness isn’t optional anymore. If your vendor says ‘we’ll get there next year,’ run. The CMS deadline isn’t a suggestion.
I hate this. All this talk about software and compliance. What about the patients who can’t afford to switch pharmacies? What about the ones who can’t even get transportation to one location, let alone choose their preferred pickup? You’re talking about perfect systems for people who already have privilege. Meanwhile, my neighbor’s 82-year-old uncle still uses a paper logbook because his Medicaid plan won’t cover e-prescribing. This isn’t progress-it’s a luxury feature for the wealthy.
Excellent breakdown. I work in a small chain in rural Ohio, and the biggest hurdle isn’t tech-it’s buy-in. Pharmacists here are skeptical of change. We rolled out PrimeRx last year. First month, staff thought it was ‘too complicated.’ Now, they won’t go back. The key? Let them see the difference in real time. One pharmacist said, ‘I didn’t realize my cousin’s prescription was being filled across town until the system flagged it.’ That’s the moment you know it works.
Also, training isn’t an expense-it’s an investment. We did 20 hours per tech. We lost two days of sales. We gained zero errors and tripled patient trust. No regrets.
LOL at the ‘philosophical’ comments. This isn’t a TED Talk, it’s a business. You want safety? Then you pay for it. No one cares about your grandma’s dignity if your pharmacy gets audited for $2M in duplicate claims. EnterpriseRx is the baseline. If you’re not using it, you’re just asking for a lawsuit.
And FHIR? You’re either on it or you’re dead. 2025 is not a suggestion. It’s a countdown. If your vendor doesn’t have a FHIR roadmap, they’re already bankrupt. Stop wasting time. Buy the software. Train the staff. Or get out.
💀🇺🇸
Y’ALL. I just saw a demo of Datascan’s AI Watchdog and I’m literally shaking. It doesn’t just flag duplicates-it predicts them. Like, it sees a pattern where someone’s filling a pain med every 3 days in three different towns and says, ‘hey, this ain’t right.’ And it doesn’t just alert-it auto-flags the prescriber for review. It’s like having a genius pharmacist watching every screen, 24/7.
I want this for my mom. I want this for my neighbor. I want this for every single senior who’s just trying to stay alive without getting poisoned by paperwork. This isn’t tech. This is love in code.
EnterpriseRx. PrimeRx. Datascan. All FHIR-compliant. If you’re not using one of these, you’re operating outside of CMS guidelines. Period. The 1.3% error rate? That’s the industry average for legacy systems. You want lower? Upgrade. You want compliance? Upgrade. You want to avoid liability? Upgrade. No debate. No nuance. Just execute.
Love the FHIR point. We’re in the middle of a transition right now and honestly? It’s messy. But the team’s been amazing. We did a pilot with two locations, let the staff give feedback, tweaked workflows, and now everyone’s on board. The key? Don’t force it. Let people feel ownership.
Also, the AI Watchdog saved us from a potential opioid diversion case last month. We didn’t even know it was happening until the system flagged it. That’s not magic-that’s smart design. Props to McKesson.
❤️
Just want to add: the hub-and-spoke model is genius. We tried going live all at once and it was chaos. Staff were overwhelmed, patients were confused, and we had two near-misses. Then we picked our flagship store as the hub-centralized all data, synced everything, and let the other locations handle clinical decisions locally. Errors dropped 38% in 3 weeks. No drama. No panic. Just smooth sailing.
Also, tell seniors they can pick up at any location. Most have no idea. My dad thought he had to go to ‘his’ pharmacy. Now he gets his meds at the one near his golf course. He’s happier. We’re happier. Win-win.
Oh my goodness, this is so important. I’m from New Orleans, and we have so many elderly folks who live alone, and their meds? Sometimes they’re just… forgotten. Or mixed up. I saw a lady last week trying to explain her pills to a pharmacist and she had them all in a Tupperware container. No labels. Just colors. I cried. This system? It’s not just tech. It’s dignity. It’s safety. It’s love. I wish every pharmacy in the country had this. Please, if you’re reading this and you manage a chain-do it. For the grandmas. For the grandpas. For the quiet ones who don’t ask for help.
Also, I think you spelled ‘prescribers’ wrong in the title? But I still love you.