Back pain can turn a normal day into an endless battle with discomfort. While pills and stretches often get mentioned, many people overlook two low‑cost, high‑impact tools: heat and cold therapy. Understanding how each works and when to apply them can dramatically speed up recovery and cut down on medication.
When we talk about Heat and Cold Therapy is a simple, non‑invasive method that uses temperature extremes to influence the body’s pain pathways and tissue health. By carefully controlling the temperature applied to a sore back, you can reduce inflammation, promote blood flow, relax tight muscles, and reset nerve signals that cause chronic pain. Below, we break down the science, the practical steps, and the safety rules you need to get real backache relief without a prescription.
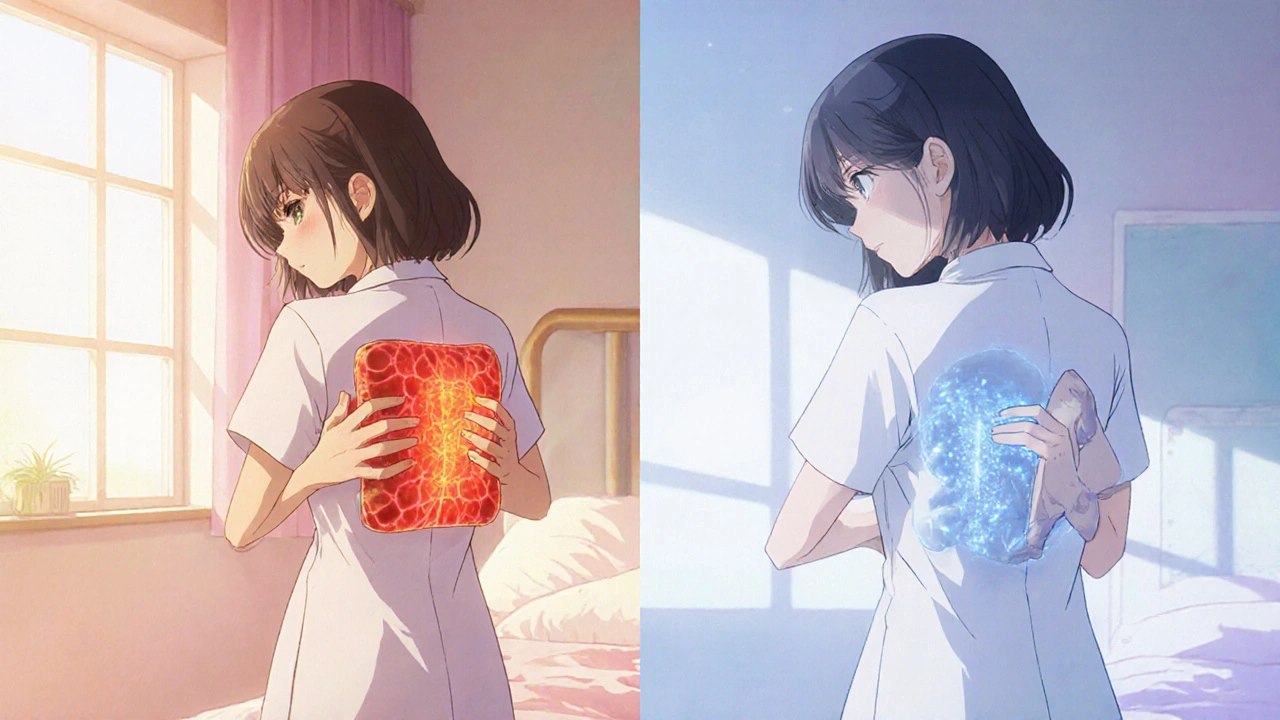
How Heat Therapy Alleviates Back Pain
Heat works primarily by expanding blood vessels, a process called vasodilation. More blood means more oxygen and nutrients reach the injured area, which speeds up the healing cascade. In addition, warmth relaxes the contractile proteins in muscle fibers, easing spasms that often lock the spine in a painful position.
Back Pain is a symptom that arises when nerves, muscles, or joints are irritated. Applying heat typically targets the muscular component of back pain, especially when the discomfort stems from chronic strain or a lingering muscle spasm.
Key attributes of effective heat therapy:
- Temperature range: 104-113°F (40-45°C) for most adults.
- Duration: 15-20 minutes per session, up to three times a day.
- Form: Moist heat (e.g., warm towel, hydro‑collar) is often more penetrating than dry heat (e.g., electric heating pad).
How Cold Therapy Calms Acute Back Injuries
Cold therapy, or cryotherapy, reduces blood flow through vasoconstriction. This limits swelling and numbs the nerve endings, which dulls the pain signal that the brain receives. It’s especially useful in the first 24‑48 hours after an acute injury such as a sudden twist or a fall.
Ice Pack is a reusable gel pack that can be chilled in a freezer for 30 minutes before use. When placed on a sore spot, the ice draws heat away from the tissue, lowering the local temperature to 40-50°F (4-10°C).
Essential cold‑therapy parameters:
- Temperature range: 40-50°F (4-10°C).
- Duration: 10-15 minutes per session, with at least a 20‑minute break between applications.
- Form: Ice packs, frozen peas, or a cold compress wrapped in a thin towel to avoid frostbite.
When to Choose Heat, When to Choose Cold
The biggest mistake people make is using heat on a fresh injury or cold on a chronic muscle spasm. Here’s a quick decision guide:
- First 24‑48 hours after trauma: Use cold therapy to control swelling.
- After the initial swelling subsides (48‑72 hours): Switch to heat to improve circulation and relax muscles.
- Chronic, dull ache with stiffness: Start with heat; add a brief cold burst if you notice swelling after activity.
- Stiffness that worsens with movement: Apply moisture heat before gentle stretching.
Remember, the goal isn’t to stay in one temperature zone all day. Alternating can be especially effective for conditions like Chronic Lower Back Pain, where inflammation and muscle tension coexist. A 20‑minute heat session followed by a 10‑minute cold compress can create a “pump‑and‑drain” effect that clears out metabolic waste while delivering fresh blood.
Practical Application Tips
Below are step‑by‑step instructions that work for most adults. Adjust the timings if you have a known sensitivity to temperature.
- Gather your tools: a heating pad or warm towel, a reusable ice pack, a thin towel or cloth.
- Test the temperature on the back of your hand. It should feel warm but not scalding, or cold but not painfully icy.
- Place the heat source directly on the painful area. If using a towel, keep it moist for deeper penetration.
- Set a timer for 15‑20 minutes. Avoid falling asleep with a heating pad on.
- After the heat session, if you need to reduce lingering inflammation, apply the ice pack for 10 minutes, wrapped in a towel.
- Gentle movement: follow each session with 5‑10 minutes of light stretching or walking to keep the muscles active.
For people who travel often, a Heat Pack that plugs into a USB port or a portable gel cold pack can be a game‑changer. These gadgets maintain therapeutic temperatures without electricity, making them ideal for office desks or road trips.
Safety Precautions You Must Observe
Temperature therapy feels safe, but misuse can cause skin burns, frostbite, or exacerbate certain medical conditions.
- Skin integrity: Never apply heat or cold directly on open wounds, rashes, or areas with reduced sensation (e.g., diabetic neuropathy).
- Duration limits: Stick to the recommended time frames. Prolonged heat can cause inflammation; excessive cold can lead to tissue damage.
- Pregnancy: Women in the third trimester should avoid heat on the abdominal area and consult a doctor before using heat on the back.
- Cardiovascular issues: Those with hypertension or heart disease should discuss temperature therapy with a physician, as extreme heat can raise heart rate.

Heat vs Cold: Quick Comparison
| Aspect | Heat Therapy | Cold Therapy |
|---|---|---|
| Primary Effect | Vasodilation, muscle relaxation | Vasoconstriction, numbness |
| Ideal Timing | After 48‑72 hrs post‑injury, chronic stiffness | First 24‑48 hrs after trauma, acute swelling |
| Typical Temp | 104‑113°F (40‑45°C) | 40‑50°F (4‑10°C) |
| Session Length | 15‑20 min, up to 3×/day | 10‑15 min, 1‑2×/day |
| Best For | Muscle spasms, chronic dull ache | Inflammation, sharp acute pain |
Frequently Asked Questions
Can I use a hot shower instead of a heating pad?
A hot shower provides moist heat similar to a warm towel, but be careful not to stay under scalding water for too long. Keep the water around 104‑110°F and limit exposure to 15 minutes.
Is it safe to combine heat and cold in one session?
Yes, alternating can be effective. Start with 15 minutes of heat, rest 5 minutes, then apply cold for 10 minutes. Make sure the skin returns to normal temperature between switches.
How often should I repeat therapy for chronic lower back pain?
Most experts recommend a daily routine: heat in the morning to loosen muscles, cold after activity that provokes soreness. Adjust based on how your body reacts.
What if I have sensitive skin or a condition like eczema?
Use a thin cloth barrier between the pack and skin, and keep the temperature at the lower end of the recommended range. If irritation occurs, stop immediately and consult a dermatologist.
Can temperature therapy replace medication for back pain?
It can reduce reliance on meds for many people, but it isn’t a universal substitute. Use it alongside prescribed treatments and discuss any changes with your healthcare provider.
Are there any long‑term risks of using heat or cold regularly?
When used correctly, the risks are minimal. Overheating can cause skin burns; excessive cold can lead to frostbite. Follow the time limits and keep a barrier between the pack and skin.
By mastering the when, how, and why of heat and cold therapy, you give your back a powerful, drug‑free ally. Try the guidelines above, listen to your body, and you’ll likely notice less pain, more mobility, and a quicker return to the activities you love.


Comments
Listen up, folks – you can’t just slap a heating pad on your back and expect miracles. The key is timing: cold when the injury is fresh, heat once the swelling calms down.
If you jump to heat within the first 24 hours you’re basically feeding the inflammation.
And don’t forget the temp range – anything above 115°F can scorch you, and nobody wants that drama! It’s definately a recipe for disaster.
Sure, because who doesn’t love a good burn, right? Just keep it simple: ice for the first two days, then switch to a warm towel. No rocket science here.
Frankly, the American healthcare system would love to dump this cheap, effective combo on patients to cut costs. Heat and cold therapy are backed by robust physiotherapy literature, yet insurers treat them like fringe hacks. By integrating thermotherapy protocols into standard PT regimens, we can reduce opioid reliance and boost functional outcomes across the nation.
Haha, love the sarcasm, but seriously, if you’re gonna toss a heating pad on, at least do it with a smile 😏. Remember to wrap that ice pack in a thin towel – we don’t need frostbite drama. You got this, stay motivated! 💪
When it comes to managing back pain, the physiological mechanisms behind temperature therapy are worth unpacking in detail. First, consider vasodilation: applying heat raises the local tissue temperature, which relaxes smooth muscle fibers and enlarges blood vessels, thereby delivering oxygen, glucose, and anti‑inflammatory mediators to the damaged area. This increased perfusion not only accelerates metabolic waste removal but also helps reset the nociceptive signaling pathways that often become hypersensitive after chronic strain. Second, the analgesic effect of heat is mediated by the activation of thermoreceptors, which send competing signals to the spinal cord, effectively “closing the gate” on pain transmission in accordance with the gate control theory. On the flip side, cold therapy initiates vasoconstriction, which limits the extravasation of plasma proteins and reduces edema formation during the acute inflammatory phase. The reduced temperature also dampens the firing rate of A‑delta and C‑fibers, providing a numbing sensation that can be especially beneficial in the first 24‑48 hours post‑injury. Additionally, cryotherapy triggers a reflex sympathetic response that can decrease muscle spasm intensity, further easing discomfort. It’s essential to respect the recommended exposure windows – typically 10‑15 minutes for cold and 15‑20 minutes for heat – because overstimulation can paradoxically exacerbate inflammation or cause tissue damage. Moreover, alternating between heat and cold creates a “pump‑and‑drain” effect, where heat expands vessels to drive blood in, and subsequent cold constricts them to push metabolic waste out, promoting a more efficient healing environment. From a practical standpoint, portable USB‑powered heat packs and reusable gel ice packs make adherence to these protocols feasible for office workers and travelers alike. Safety considerations remain paramount: always place a barrier such as a thin cloth between the pack and skin, monitor skin color and temperature, and avoid therapy on areas with compromised sensation, such as diabetic neuropathy. Finally, integrating temperature therapy with gentle movement – a brief session of stretching or walking after each application – can prevent stiffness and reinforce the benefits of improved circulation. In summary, a disciplined, evidence‑based approach to heat and cold therapy can dramatically reduce reliance on pharmacologic analgesics, enhance functional recovery, and empower patients to take active control over their back health.
To add a technical layer, the concept of thermally induced phase change in collagen fibers explains why heat facilitates tissue remodeling – the denaturation threshold of collagen lies around 60°C, but therapeutic heat stays well below that, promoting pliability without degradation. Meanwhile, cryotherapy modulates the inflammatory cascade by attenuating cytokine release such as interleukin‑1β and tumor necrosis factor‑α, which are pivotal in the early post‑injury phase. Aligning these molecular insights with the clinical protocol you outlined maximizes therapeutic efficacy.
Bottom line – if you’re still in pain after a week, stop messing around and stick to the schedule: ice then heat, don’t overdo either, and add a few minutes of movement. Your back will thank you.
While your directness is noted, it would be prudent to acknowledge the individual variability in response to thermotherapy, especially among patients with cardiovascular comorbidities. A measured approach respecting clinical guidelines ensures safety and efficacy.
Think of your back like a garden; a warm sun‑shower after the frost helps the seedlings grow, but too much heat wilts them. Mix the warmth with a cool mist when the soil’s soggy, and you’ll see the blossoms of mobility return.
Got it 😊. I’ll try the heat‑then‑ice routine after my morning stretch.
Will give it a shot tomorrow.