More than 1 in 4 adults worldwide have fat building up in their liver - not from drinking alcohol, but from how they eat, move, and live. This isn’t just about being overweight. It’s a metabolic problem called MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease), the new name for what used to be called NAFLD. And it’s getting worse. In the UK alone, over 9 million people are estimated to have it. The good news? You can reverse it. The better news? Weight loss and newer medications like GLP-1 agonists are changing the game.
What Actually Happens in Your Liver When You Have MASLD?
Your liver isn’t just filtering toxins - it’s also managing your body’s energy. When you eat more calories than you burn, especially from sugar and refined carbs, your liver starts turning that extra energy into fat. Normally, it stores it safely. But when insulin resistance kicks in - which happens with obesity, prediabetes, or high blood pressure - your fat cells start leaking fatty acids into your bloodstream. About 59% of the fat that piles up in your liver comes from these leaked fats. Another 26% is made right inside your liver from the carbs you eat. Your liver can’t burn or export it fast enough, so it just sits there.
At first, it’s just fat. That’s steatosis. But if it keeps going, inflammation shows up. Immune cells attack the fat-filled liver cells. Scar tissue begins to form. That’s MASH - the more dangerous stage. Left unchecked, it can lead to cirrhosis or liver cancer. And here’s the scary part: most people don’t feel anything until it’s advanced. No pain. No jaundice. Just a silent buildup.
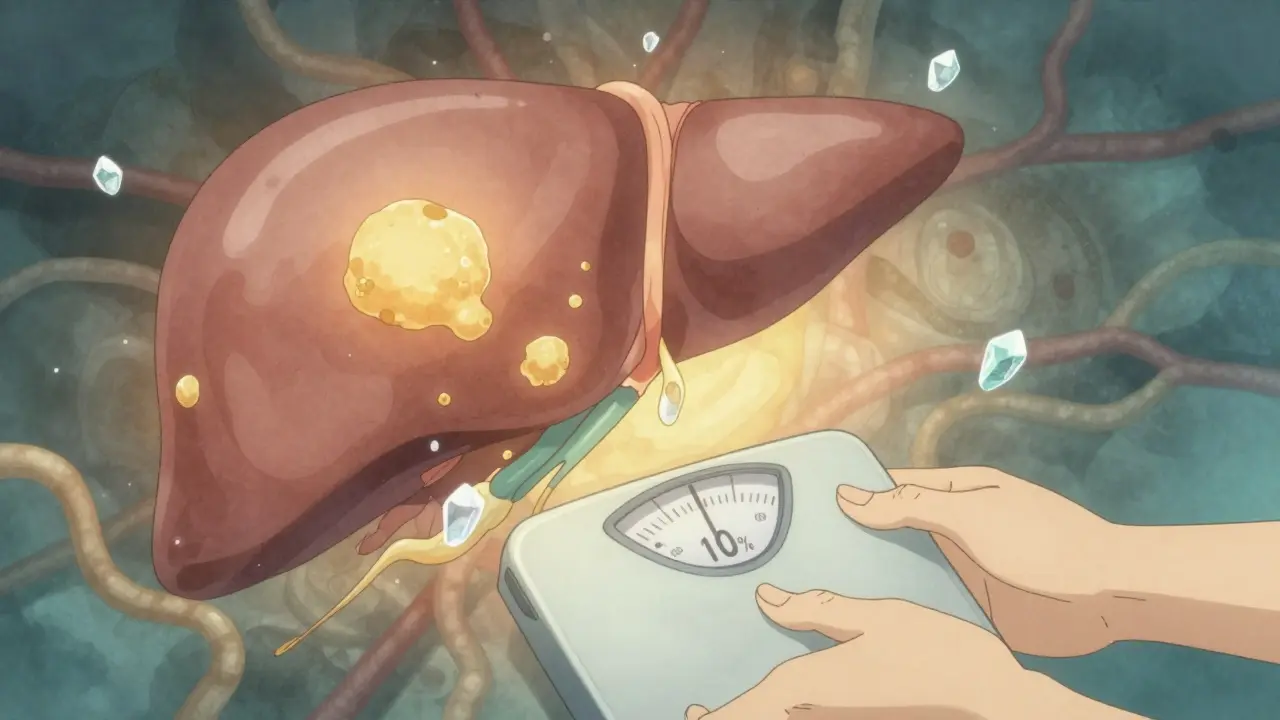
Why Losing Weight Isn’t Just About Looking Better
Weight loss isn’t a suggestion - it’s the most proven treatment we have. But not just any weight loss. Losing 5% of your body weight? That helps reduce liver fat. But if you want to reverse inflammation and early scarring, you need to hit 10% or more.
Studies show that people who lost 10% of their body weight through diet and exercise had a 45% chance of completely clearing MASH. In the Look AHEAD trial, those who stuck with intensive lifestyle changes cut their risk of developing MASH by 90% compared to those who didn’t. How? Because losing weight cuts the flood of fatty acids from your belly fat to your liver by 30-40%. It also turns down the dial on your liver’s own fat-making machine by 25-35%. Your liver starts burning fat again instead of hoarding it.
It’s not magic. It’s math. You need to create a calorie deficit. The European Association for the Study of the Liver recommends 1,200-1,800 calories a day, depending on your size, and at least 150 minutes of brisk walking or cycling each week. Mediterranean diets - full of vegetables, olive oil, fish, nuts, and whole grains - work better than low-fat diets for liver health. Cut out sugary drinks. Fructose is the worst offender. Just 25 grams a day (about one can of soda) can worsen liver fat.
GLP-1 Drugs: More Than Just Weight Loss Pills
For many people, losing 10% of their body weight through diet and exercise alone is nearly impossible. That’s where GLP-1 receptor agonists come in. These aren’t just weight loss drugs - they’re metabolic reset buttons.
Semaglutide (Wegovy®, Ozempic®) and liraglutide (Saxenda®) were originally designed for type 2 diabetes. But they do something remarkable: they make you feel full faster, slow down digestion, and reduce cravings. In the STEP-1 trial, people on semaglutide lost an average of 15% of their body weight. In the same group, liver fat dropped by 55% - measured by MRI, not guesswork.
But it’s not just about weight. These drugs act directly on the liver. They turn off the fat-making pathway (de novo lipogenesis) by activating AMPK, a natural cellular brake. They reduce inflammation by blocking NF-κB, a key trigger for liver damage. In the REGENERATE trial, 52% of patients on semaglutide saw MASH resolve after 72 weeks. Only 22% did on placebo. That’s not a small difference - that’s a game-changer.
Liraglutide did something similar in the SCALE trial: 39% of patients cleared MASH, compared to just 17% on sugar pills. These aren’t theoretical results. They’re backed by liver biopsies and MRI scans - the gold standard.

The Catch: Side Effects and Sticking With It
These drugs work - but they’re not easy to tolerate. About 76% of people on semaglutide report nausea. Some get vomiting, diarrhea, or constipation. In real-world settings, nearly a third quit within six months because of it.
One patient on Reddit, ‘LiverWarrior42’, shared that after nine months on semaglutide, they lost 12.3% of their weight and saw their liver fat score drop from 328 to 245 on FibroScan. But they also said the first month felt like being sick every day. They started taking vitamin B6 (pyridoxine), which helped. Others found slow titration - starting at the lowest dose and increasing every 4 weeks - made the side effects manageable.
Adherence is the biggest hurdle. When people get counseling along with the drug, 65% stick with it after a year. Without it, only 42% do. That’s why clinics like Duke’s MASLD program pair medication with weekly dietitian visits for the first three months. Meal replacement shakes helped 78% of patients stick to their plan. Just telling someone to eat better doesn’t cut it.
Who Gets These Drugs - And Who Doesn’t?
Right now, GLP-1 agonists are approved for weight loss (Wegovy®) and type 2 diabetes (Ozempic®). But insurance coverage varies wildly. In the US, Medicare covers about two-thirds of people for obesity, but in the UK, NHS access is still limited. Private prescriptions cost around £1,200-£1,350 a month. That’s out of reach for most.
They’re not for everyone. If you already have advanced scarring (F3-F4 fibrosis), GLP-1 drugs alone won’t fix it. That’s where new drugs like resmetirom - approved in early 2024 - may come in. It targets liver fat directly and is being tested in combination with semaglutide. Early data suggests it could help people who’ve plateaued.
And while these drugs reduce heart attacks and strokes in people with obesity and MASLD (as shown in the SELECT trial), they’re not a magic shield. You still need to move, eat well, and sleep enough. The drugs help you get there - but they don’t replace the foundation.

What’s Next for MASLD Treatment?
The landscape is changing fast. In 2023, the FDA started accepting MRI scans and FibroScan readings as proof of improvement in drug trials - meaning new treatments can be approved faster. The global market for MASLD drugs is expected to hit $28 billion by 2030. Semaglutide leads, but tirzepatide (Mounjaro®) is coming up fast - it’s even more effective at weight loss.
But the real challenge isn’t the science. It’s access. Only 28% of rural counties in the US have a specialist who knows how to manage MASLD. In the UK, most GPs still don’t screen for it. Blood tests like FIB-4 and FibroScan are cheap and non-invasive - yet rarely ordered unless liver enzymes are sky-high.
What’s clear: MASLD is no longer a side effect of obesity. It’s a core metabolic disease. And the treatment isn’t just about shrinking your waistline - it’s about healing your liver. Weight loss is the foundation. GLP-1 drugs are the accelerator. Together, they’re turning a silent epidemic into a treatable condition.
What You Can Do Today
- If you’re overweight or have type 2 diabetes, ask your doctor for a FibroScan or FIB-4 blood test. Don’t wait for symptoms.
- Start with a 5% weight loss goal. Use a food tracker. Cut out sugary drinks. Add 30 minutes of walking daily.
- If you’re struggling to lose weight, ask about GLP-1 agonists. Not everyone qualifies, but it’s worth discussing.
- Don’t stop at the scale. Ask for liver fat testing (MRI-PDFF or FibroScan) before and after 6-12 months. That’s how you know if it’s working.
- Join a support group. Whether it’s online or in person, people who stick with treatment have better outcomes.
This isn’t about perfection. It’s about progress. One less soda. One extra walk. One conversation with your doctor. Those small steps add up - and they can save your liver.
Is MASLD the same as NAFLD?
No. NAFLD was defined by what it wasn’t - no alcohol, no other liver disease. MASLD is defined by what it is: fat in the liver plus at least one metabolic issue like obesity, high blood sugar, or high blood pressure. This change means doctors now diagnose it positively, not by ruling things out. It’s more accurate and catches more people who need help.
Can you reverse MASLD without medication?
Yes - but only if you lose enough weight. Losing 5-7% of your body weight reduces liver fat. Losing 10% or more can reverse inflammation and early scarring. Studies show 45% of people who hit that 10% goal clear MASH entirely. Diet and exercise alone work - but they’re hard to sustain. That’s why many people need help.
Do GLP-1 drugs cure fatty liver?
They don’t ‘cure’ it, but they can reverse the most dangerous stages. In clinical trials, 52% of people on semaglutide saw MASH resolve. That means the inflammation and cell damage went away. But if you stop the drug and gain weight back, the fat and inflammation can return. It’s a treatment, not a one-time fix.
Are GLP-1 drugs safe for the liver?
Yes - they’re actually good for it. Early concerns about liver injury were unfounded. In fact, these drugs reduce liver fat, inflammation, and even fibrosis. The main risks are gastrointestinal side effects like nausea, not liver damage. Rare cases of pancreatitis have been reported, but the risk is less than 0.3% per year.
How long do you need to take GLP-1 drugs for fatty liver?
There’s no fixed timeline. Most studies show benefits after 72 weeks (about 1.5 years). But because MASLD is a chronic metabolic condition, stopping the drug often leads to weight regain and liver fat returning. Think of it like blood pressure medication - you take it as long as you need to manage the condition. Some people may eventually taper off after sustained weight loss and lifestyle changes, but many will need long-term support.
Can I take GLP-1 drugs if I don’t have diabetes?
Yes. Semaglutide (Wegovy®) and liraglutide (Saxenda®) are approved specifically for weight loss in people without diabetes. You don’t need to have type 2 diabetes to qualify. The key criteria are BMI ≥30 (or ≥27 with weight-related health issues) and evidence of MASLD. Always check with your doctor - eligibility depends on local guidelines and insurance.

Comments
Okay but let’s be real - if you’re drinking one soda a day, you’re basically pouring sugar directly into your liver. I cut out soda last year and my FibroScan dropped 40 points in six months. No drugs. Just water, walking, and saying no to the vending machine at work. It’s not sexy, but it works.
Look, I get the hype around GLP-1s - they’re basically metabolic magic bullets - but let’s not pretend this is some new revelation. The liver doesn’t care if you’re on Ozempic or just ate a salad. It cares about insulin resistance, visceral fat, and fructose overload. The drugs help you get there, sure, but they’re not a substitute for metabolic literacy. People think popping a pill lets them go back to eating processed crap. That’s not healing. That’s just chemical band-aiding a systemic collapse. The real revolution isn’t the drug - it’s the cultural shift away from ‘eat less, move more’ as a moral failing and toward understanding metabolic physiology as a biological reality. And honestly? Most doctors still don’t get it.
Interesting data, but where’s the long-term follow-up? 72 weeks is nothing in the context of a chronic disease. Also, 52% resolution on semaglutide? That’s impressive - but what about the other 48%? Did they just get worse? And how many of those ‘resolved’ cases relapsed after stopping? The trials are funded by pharma. Always check the funding. 🤔
As a registered dietitian who specializes in metabolic health, I can confirm: the 10% weight loss threshold is the golden number for MASH reversal. But what’s rarely discussed is the role of protein timing and circadian rhythm. Eating your largest meal before 3 PM and getting 1.6g/kg of protein daily improves hepatic insulin sensitivity independently of total calories. Also - magnesium deficiency is rampant in MASLD patients. Don’t ignore the micronutrients. And yes, B6 helps with nausea - that’s legit. Many patients don’t know that.
While the data presented is statistically significant, one must consider the selection bias inherent in clinical trials. Participants are highly motivated, closely monitored, and often receive nutritional counseling - conditions not replicable in the general population. Moreover, the cost-benefit analysis of GLP-1 agonists remains questionable, especially in resource-limited settings. One cannot ethically advocate for a treatment that is inaccessible to 90% of those who need it. The real solution lies in public health policy, not pharmaceutical innovation.
My mom was diagnosed with MASLD last year. She started walking 45 minutes every morning, swapped soda for sparkling water with lemon, and took liraglutide after her doctor pushed for it. She lost 14% of her body weight. Her liver enzymes went from 120 to 38. She cried when she saw the FibroScan results. It’s not just about health - it’s about being able to play with her grandkids without getting winded. I’m so glad she didn’t wait for ‘something worse’ to happen.
Wait - so if I just take Wegovy, I can eat pizza every night and still reverse my fatty liver? That’s the message people are getting. And now everyone’s on it. I saw a guy at the gym on Ozempic doing 10 reps with 50lbs while eating a whole bag of chips. Bro, that’s not a reset - that’s a disaster waiting to happen. The drug is not a license to be lazy.
It is utterly irresponsible to promote GLP-1 agonists as a primary intervention for a metabolic condition that is fundamentally rooted in lifestyle. The medicalization of personal responsibility is a dangerous precedent. One does not cure chronic disease with a prescription - one cures it with discipline, restraint, and moral fortitude. The fact that we have reduced complex human behavior to a pharmacological fix speaks volumes about the decay of our cultural values.
For anyone feeling overwhelmed - you’re not alone. I was diagnosed with MASLD at 38, and I thought my liver was a goner. I started with one walk a day. Then I swapped soda for herbal tea. Then I joined a free online support group. Six months later, I lost 8%. I didn’t need a drug. I needed someone to say, ‘Hey, you got this.’ If you’re reading this and you’re scared - you’re not broken. You’re just early in the journey. One step. One day. One less soda. You’ve already won.
Bro, I lost 16% on semaglutide. First month was hell - nausea, dizziness, felt like I was dying. Then I started taking B6 and went slow with the dose. Now I feel better than I have in 15 years. My wife says I’m not as grumpy. 😅 My liver scan? Normal. I’m not a ‘cured’ person - I’m a ‘managed’ person. And that’s okay.
The normalization of GLP-1 agonists as weight-loss tools is emblematic of the broader commodification of health in late-stage capitalism. The conflation of metabolic health with aesthetic outcomes - ‘slimmer waist, better liver’ - reduces a complex pathophysiological condition to a cosmetic concern. One wonders whether the real agenda is not healing, but market expansion. The pharmaceutical-industrial complex thrives on chronicity, not cure.
I’m a nurse. I’ve seen patients cry because they can’t afford Ozempic. I’ve seen others stop because they couldn’t handle the side effects. I’ve seen others lose weight and go right back to their old habits because no one taught them how to cook. This isn’t just about medicine. It’s about access, education, and compassion. We need more community health workers, not just prescriptions.
Let’s not romanticize weight loss. Many of us have tried. Many of us have failed. The real issue isn’t willpower - it’s the food environment. Fast food is cheaper than broccoli. Sugar is everywhere. And now we’re blaming people for being victims of a broken system? GLP-1 drugs are a band-aid on a bullet wound. We need food policy reform. We need subsidies for vegetables. We need to ban sugar advertising to kids. Until then, telling people to ‘just lose weight’ is cruel.