Low‑Density Lipoprotein is a lipoprotein that transports cholesterol from the liver to peripheral tissues, commonly referred to as "bad cholesterol" because high levels are linked to atherosclerosis. Osteoporosis is a systemic skeletal disease characterized by low bone mineral density (BMD) and structural deterioration, leading to increased fracture risk. While most people think of LDL only in heart‑health terms, recent research shows it also talks to bone cells. This article untangles the connection, backs it with clinical data, and gives you a clear‑cut plan to keep both your arteries and skeleton in shape.
Quick Takeaways
- Elevated LDL can accelerate bone loss by promoting inflammation and disrupting calcium balance.
- Statin therapy may improve bone mineral density, but benefits depend on dose and patient age.
- VitaminD, calcium, and regular weight‑bearing exercise offset many LDL‑related bone risks.
- Regular lipid panels and bone density scans together give a fuller picture of health.
- Managing cholesterol is a dual‑win: it protects the heart and may preserve bone strength.
What Low‑Density Lipoprotein Does in the Body
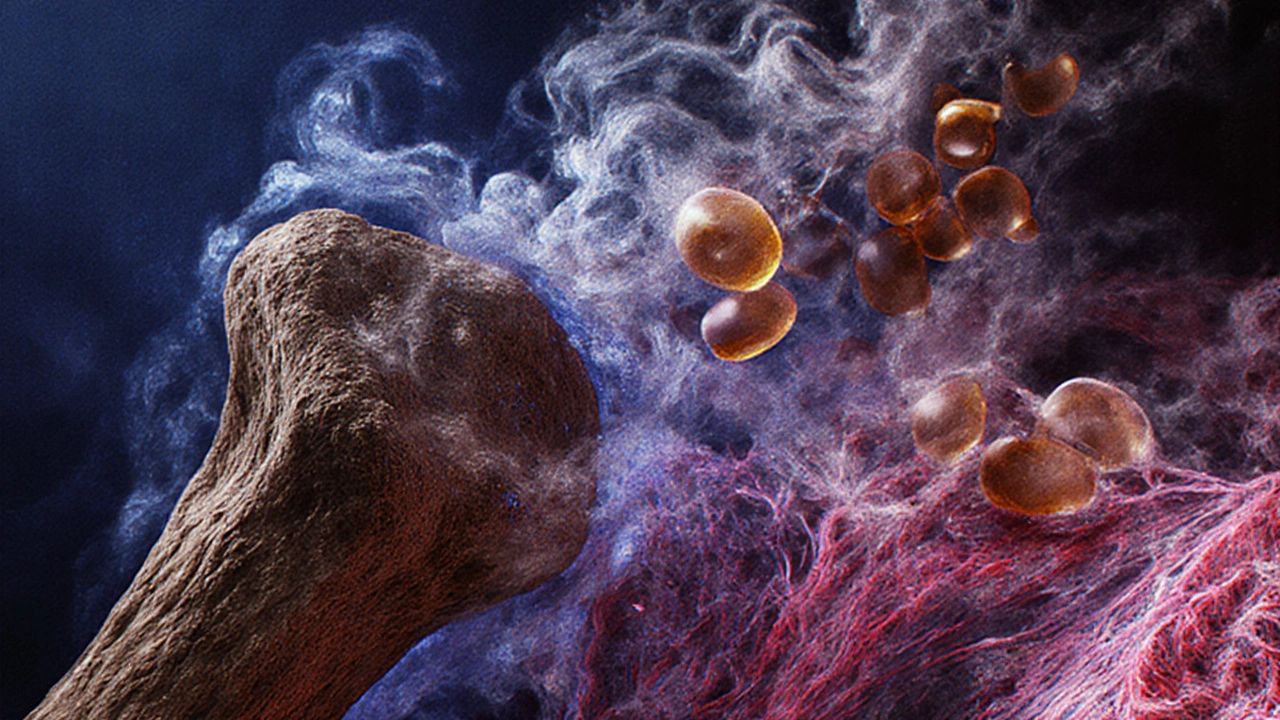
LDL particles cholesterol a waxy substance essential for cell membrane integrity and hormone synthesis travel through blood vessels, delivering lipid cargo to cells that need it. When LDL is oxidized (oxLDL), it triggers inflammatory cytokines signalling proteins like IL‑6 and TNF‑α that promote inflammation. These cytokines are the same messengers that stimulate bone‑resorbing cells.
Understanding Osteoporosis and Its Main Players
Bone is a living tissue, constantly remodeled by two opposing cell types: osteoclasts cells that break down bone matrix and osteoblasts cells that form new bone. The balance between them determines bone mineral density the amount of mineral (mainly calcium phosphate) per volume of bone. When remodeling tips toward resorption, BMD drops, raising the fracture risk the probability of breaking a bone during everyday activities.
How LDL Influences Bone Health
Three key pathways link high LDL to weaker bones:
- Inflammation - oxLDL activates the NF‑κB pathway, increasing IL‑6 and TNF‑α. These cytokines boost osteoclast activity while suppressing osteoblast formation, directly lowering BMD.
- Calcium Competition - LDL receptors on intestinal cells can compete with calcium transporters, reducing dietary calcium absorption. Lower serum calcium triggers parathyroid hormone a hormone that raises blood calcium by pulling it from bone, further stimulating bone loss.
- Lipid Deposition in Bone Marrow - Excess fat in the marrow creates a hostile environment for osteoblasts and encourages adipocyte differentiation, a state seen in both osteoporosis and metabolic syndrome.
These mechanisms are not theoretical. Studies on post‑menopausal women show a linear correlation: each 10mg/dL rise in LDL corresponds to a 0.3% drop in lumbar spine BMD.

Clinical Evidence Linking LDL and Osteoporosis
Large‑scale cohort studies from the US and Europe provide real‑world data:
- The Framingham Osteoporosis Study a 20‑year follow‑up of 4,500 adults reported that participants in the highest LDL quartile had a 1.7‑fold higher odds of a hip fracture after adjusting for age, smoking, and BMI.
- A meta‑analysis of 12 randomized controlled trials (RCTs) found that statin cholesterol‑lowering drugs that inhibit HMG‑CoA reductase users gained an average of 2.1% in femoral neck BMD compared with placebo.
- Conversely, a British cohort of 3,200 men showed that low HDL (the "good" cholesterol) did not have a clear protective effect on bone, reinforcing that LDL is the main lipid culprit.
These findings suggest a bidirectional relationship: managing LDL not only shields the heart but may also blunt bone loss.
Nutrition, Lifestyle, and Medication Strategies
Below is a practical toolbox that addresses both cholesterol and bone health.
| Intervention | Primary Effect on LDL | Impact on BMD | Key Considerations |
|---|---|---|---|
| Statin Therapy | ↓30-50% LDL | ↑1-3% BMD (dose‑dependent) | Monitor liver enzymes; best for ages50+ |
| Plant‑Sterol Enriched Foods | ↓10% LDL | Neutral | Easy daily incorporation; limited effect on bone |
| Weight‑Bearing Exercise | Neutral | ↑2-4% BMD | 30min, 3‑5times/week; also lowers LDL modestly |
| VitaminD+Calcium Supplementation | Neutral | ↑1-2% BMD | Ensure 800-1,000IU D3 & 1,200mg Ca daily |
| Low‑Carb, High‑Sat Fat Diet | ↑ LDL | ↓ BMD | Avoid; raises both heart and bone risk |
Notice how statins are the only drug that simultaneously hits LDL and boosts BMD. However, not everyone tolerates statins, so lifestyle choices become crucial.
Checklist: Protecting Your Heart and Bones
- Get a fasting lipid panel and a DXA scan at least every 2years after age50.
- Aim for LDL<100mg/dL (or <70mg/dL if you have cardiovascular disease).
- Consume ≥1,200mg calcium and 800-1,000IU vitaminD daily; check serum 25‑OH‑D.
- Fit in weight‑bearing activity-walking, jogging, resistance training-for ≥150minutes weekly.
- Limit saturated fat to <7% of total calories; replace with polyunsaturated fats (olive oil, nuts).
- Discuss statin eligibility with your GP, especially if you have osteoporosis or a family history of fractures.
Related Concepts and Next Steps
Understanding the LDL‑osteoporosis link opens doors to deeper topics. You may want to explore:
- Inflammaging the chronic low‑grade inflammation that increases with age and its impact on both heart and bone.
- The role of estrogen replacement therapy hormone therapy that can raise HDL and protect bone in post‑menopausal women.
- How bone turnover markers biochemical indicators like CTX and P1NP can track treatment response.
- Emerging therapies such as PCSK9 inhibitors and their unknown effects on bone density.
Each of these areas deepens the picture of how our metabolic systems interconnect. Keep an eye on new research-today’s cholesterol‑focused drug could be tomorrow’s bone‑preserving breakthrough.
Frequently Asked Questions
Does high LDL directly cause osteoporosis?
High LDL contributes to bone loss mainly through inflammatory pathways and calcium competition. It’s not the sole cause-age, hormones, and nutrition also play big roles-but lowering LDL can reduce one of the key risk factors.
Can taking statins replace calcium supplements?
No. Statins may modestly improve bone density, but calcium and vitaminD remain essential for forming new bone. Use statins for cholesterol control and keep the traditional bone‑support regimen.
How often should I have my LDL and bone density checked?
If you’re over 50 or have risk factors, a fasting lipid panel every 1‑2years and a DXA scan every 2years are reasonable. High‑risk individuals may need annual monitoring.
Is a low‑carb diet safe for bone health?
Low‑carb diets can be okay if they include plenty of leafy greens, nuts, and dairy to supply calcium and vitaminD. The bigger danger is excessive saturated fat, which spikes LDL and can harm bone.
Do women need to worry more about LDL‑related bone loss?
Yes, post‑menopausal women lose estrogen, which normally protects both cholesterol levels and bone. Managing LDL becomes even more critical to offset the accelerated bone turnover.


Comments
High LDL isn’t just a heart‑enemy; it actively fuels the inflammation that drives bone‑resorbing cells. If you skip regular lipid panels, you’re basically signing up for weaker bones and higher fracture risk.
So you think cholesterol only matters for arteries? Think again-your blood is a battlefield and LDL is the rogue soldier attacking both heart and skeleton.
LDL spikes = more oxLDL = cytokine storm = osteoclast overdrive. Statins help, but diet and weight‑bearing moves are non‑negotiable.
Thank you for outlining the mechanistic pathways so clearly. The interplay between lipid metabolism and bone remodeling is indeed a fascinating frontier, and your checklist provides a pragmatic roadmap for clinicians and laypersons alike.
I appreciate the thoroughness, especially the emphasis on regular DXA scans alongside lipid panels. Integrating both assessments can truly give a holistic picture of an individual’s health trajectory.
While the casual reader may dismiss LDL as merely a cardiovascular culprit, the biochemical literature substantiates a far more intricate nexus with skeletal homeostasis. Oxidized LDL, for instance, precipitates the activation of NF‑κB, a transcription factor that upregulates pro‑inflammatory cytokines such as IL‑6 and TNF‑α. These cytokines, in turn, potentiate osteoclastogenesis by enhancing RANKL expression on osteoblast lineage cells. Moreover, the competitive inhibition of calcium transporters by LDL receptors in enterocytes can attenuate dietary calcium absorption, thereby eliciting a secondary hyperparathyroid response that mobilizes calcium from bone reservoirs. The adipogenic drift observed within the bone marrow niche under conditions of hyperlipidemia further exacerbates osteoblast suppression, as mesenchymal stem cells preferentially differentiate into adipocytes. Empirical evidence from the Framingham Osteoporosis Study demonstrates a statistically significant association between LDL quartiles and hip fracture incidence, even after adjusting for confounders such as age, smoking status, and body mass index. Complementary meta‑analytic data reveal that statin therapy confers a modest yet reproducible increase in femoral neck bone mineral density, highlighting a pharmacologic avenue that simultaneously addresses dyslipidemia and osteopenia. Nonetheless, the dose–response relationship remains nuanced; high‑intensity statins may yield diminishing returns on bone outcomes while escalating hepatic adverse events. Dietary interventions, particularly the incorporation of plant sterols, have been shown to reduce LDL concentrations by approximately ten percent, albeit with a neutral impact on bone turnover markers. Conversely, low‑carbohydrate, high‑saturated‑fat regimens paradoxically elevate LDL and are associated with deleterious effects on bone mineral density, underscoring the importance of macronutrient balance. Weight‑bearing exercises, such as resistance training and brisk walking, exert a dual benefit by modestly improving lipid profiles and stimulating osteoblastic activity. Vitamin D and calcium supplementation remain foundational, ensuring adequate substrate availability for mineralization processes. Ultimately, a synergistic approach-integrating pharmacotherapy, nutrition, and mechanical loading-offers the most robust strategy for mitigating the intertwined risks of atherosclerosis and osteoporosis. Future randomized controlled trials should prioritize composite endpoints that capture both cardiovascular and skeletal outcomes to refine therapeutic guidelines. In sum, the dichotomy between “bad cholesterol” and bone health is a false binary; the two systems are inextricably linked, and clinicians ought to adopt a holistic perspective.
Statins may boost bone density, but they also carry muscle pain risk, which can limit exercise adherence.
One must not be fooled by simplistic claims; the lipid‑bone axis is a sophisticated symphony, and only a discerning mind appreciates its subtleties.
this stuff is sooo overcomplicated lol.
Great rundown! 👍 I’m definitely adding more weight‑bearing workouts and checking my LDL every year. 😊
Same here! 🎉 Keeping an eye on both cholesterol and bone health is the smartest move we can make.
Honestly, if you keep ignoring the link between heart and bone, you’re just courting disaster – it’s not just a medical issue, it’s a moral failure to care for your own body.