Generic drugs have long been the backbone of affordable healthcare. But the next wave isn’t just copies of old pills-it’s smarter, more complex, and harder to make. These are generic combinations: products that merge multiple active ingredients, advanced delivery systems, or modified-release technologies into a single dose. They’re not your grandfather’s generics. They’re designed to improve how patients take medicine, reduce side effects, and make treatments more effective-all while staying cheaper than brand-name drugs.
What Exactly Are Generic Combinations?
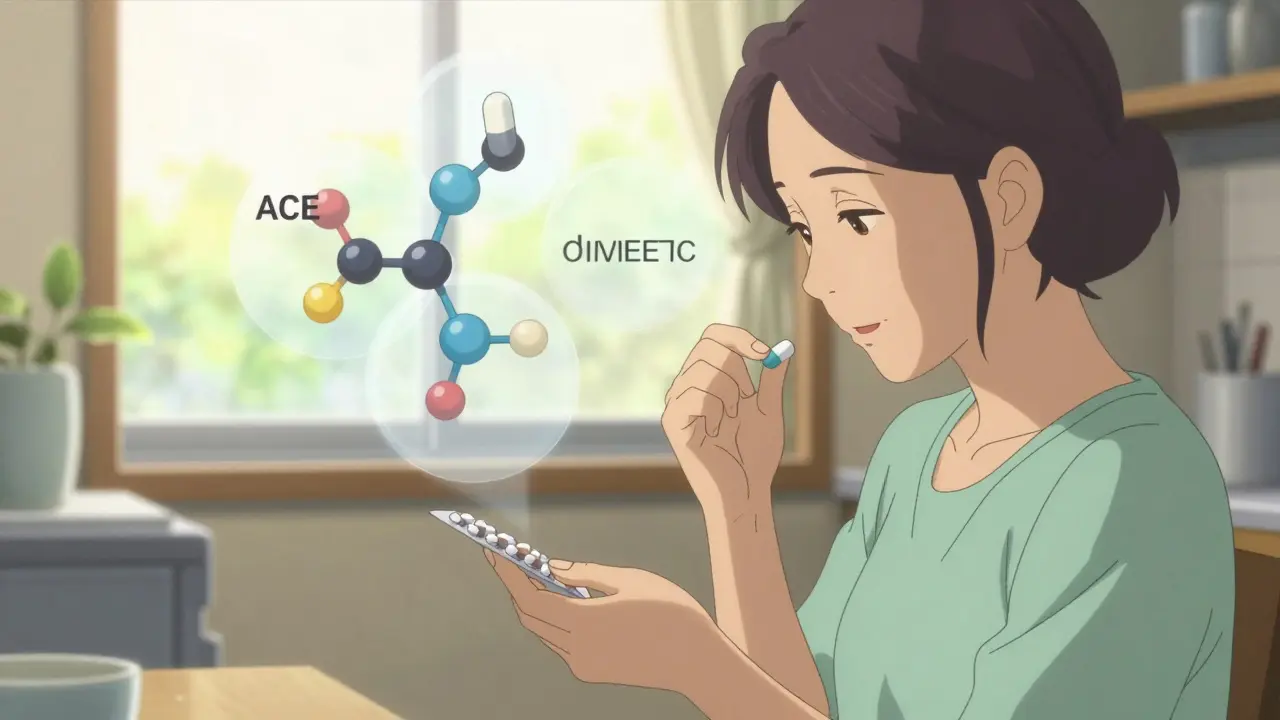
Traditional generics replicate a single active ingredient after a brand’s patent expires. Generic combinations go further. They combine two or more drugs into one pill, like a blood pressure medicine that includes both an ACE inhibitor and a diuretic. Or they add a device-think an inhaler with a built-in dose counter, or an auto-injector for diabetes meds. Some even use special coatings or materials to control how slowly the drug releases in your body.
These aren’t just convenience tweaks. They solve real problems. Patients on multiple pills often forget doses. A single combination pill cuts that risk. For conditions like asthma or depression, timing matters. Modified-release versions ensure steady drug levels, avoiding spikes and crashes. And for chronic diseases like diabetes or heart failure, better adherence means fewer hospital visits.
Why the Market Is Exploding
The global market for these advanced generics-called super generics-is set to more than double by 2035, hitting $474.6 billion. That’s a 7.2% annual growth rate. Why now? Because big patents are expiring.
Between 2025 and 2030, drugs bringing in $217-$236 billion each year will lose exclusivity. That includes blockbuster treatments like Trelegy Ellipta (for COPD), which made $2.8 billion in 2024 alone. Or Austedo, used for movement disorders, with $1.2 billion in sales. These aren’t small drugs. They’re high-value targets.
And here’s the kicker: while regular generics get crushed by price cuts-losing 80-90% of their value within two years-generic combinations hold onto 40-60% of their price for five years or more. That’s why companies like Teva, Viatris, and Aspen are pouring money into them. One extended-release version of bupropion (an antidepressant) brought in $187 million annually, while standard generics of the same drug only made $42 million combined.
Regulatory Hurdles Are Getting Tougher
Getting these products approved isn’t easy. The FDA treats them differently than plain generics. A regular generic needs to prove it’s pharmaceutically and bioequivalent to the brand. That’s straightforward. But for a combination product? You need more data. Much more.
Drug-device combos-like inhalers or injectors-require special review by the FDA’s Office of Combination Products. You have to show not just that the drug works, but that the device delivers it correctly, every time. Modified-release pills need complex pharmacokinetic studies. And fixed-dose combinations? You must prove the combo works better than taking the drugs separately.
According to FDA internal data from 2024, approval for complex combinations takes 18-24 months longer than for simple generics. And they require 30-50% more clinical data. That’s expensive. While a basic generic might cost $1-5 million to develop, a complex combination can run $15-50 million. Most small companies can’t afford it.
And it’s not just the U.S. The European Medicines Agency (EMA) is much more cautious. Through early 2025, the U.S. approved 37 complex generic combinations. The EU approved just 12. That means companies can’t assume one approval means global access. They have to tailor strategies for each region.
Who’s Winning and How
The leaders aren’t the biggest names-they’re the ones focused on complexity. Sandoz split from Novartis to become a pure-play generics company, betting everything on advanced products. Viatris and Credence merged for $2.3 billion in 2025 specifically to boost their capabilities in complex combinations.
Manufacturing is another battleground. These products need precision. A 2% error in mixing two drugs can make a difference in effectiveness. That means companies need hot-melt extrusion machines, lipid-based delivery systems, and equipment that can maintain ±2% tolerance. Only a handful of manufacturers worldwide have the tech.
India is becoming the manufacturing hub, producing 35% of the world’s complex generics. But the U.S. is pushing back. In October 2025, the FDA launched a pilot program that fast-tracks reviews for generic combinations made entirely in the U.S. That could cut approval time by 3-6 months. It’s a clear signal: the U.S. wants to keep this business homegrown.
Therapeutic Areas That Are Booming
Not all generic combinations are equal. Some areas are growing faster than others.
- Oncology: Kinase inhibitor combos are growing at 11.3% a year. These are tricky to replicate, but when done right, they can improve survival rates.
- Respiratory: Inhalable combinations for asthma and COPD are up 9.89% annually. Devices matter here-delivery accuracy is everything.
- CNS: For depression, Parkinson’s, and epilepsy, modified-release versions are in high demand. Patients need stable drug levels, not peaks and valleys.
Meanwhile, simple oral FDCs-like two pills in one tablet-are still the most common, making up 62% of volume. But they’re growing slowly (5.2% CAGR). The real money is in the complex stuff: drug-device combos and nanoparticle systems, growing at nearly 13% a year.
The Risks and the Future
There’s a dark side. Experts warn that the rules for proving these products are equivalent aren’t clear enough. Dr. Aaron Kesselheim from Harvard wrote in the New England Journal of Medicine that we’re creating safety gaps by pushing the boundaries of what counts as a “super generic.” If a modified-release pill releases drug too fast, it could cause toxicity. Too slow, and it won’t work. Without standardized testing, patients could be at risk.
And pricing pressure is rising. Even with higher margins, IQVIA predicts that if companies don’t keep innovating, all generics could face 30% margin erosion over the next decade. The market is waking up to the fact that low-cost isn’t enough anymore. Patients and payers want better outcomes.
Looking ahead, three trends are clear:
- Complexity = Premium: Products with multiple innovations-like a combo inhaler with a digital sensor-can charge 2-3 times more than regular generics.
- Regional Split: The U.S. will keep moving faster than Europe and other markets. Companies will need separate strategies for each region.
- Partnerships Are Key: Generic companies are teaming up with device makers. Catalent and Hikma are working together on auto-injectors. No one can do it alone anymore.
By 2030, super generics could make up 35-40% of the total generics market value. That’s not a niche anymore. It’s the future. Companies that stick to simple copies will keep losing money. Those that invest in smarter, more complex products will survive-and thrive.
What This Means for Patients and Providers
For patients, this means more options that are easier to use and more effective. Fewer pills. Fewer side effects. Better control of chronic conditions.
For doctors, it means having better tools to improve adherence. A single pill that combines a statin, a blood pressure med, and a low-dose aspirin? That’s a game-changer for heart disease patients.
For payers, it’s a balancing act. These products cost more upfront than plain generics. But they reduce hospitalizations, ER visits, and long-term complications. The math still works-if the system supports innovation.
What’s the difference between a generic and a generic combination?
A regular generic copies a single drug after its patent expires. A generic combination includes two or more drugs in one dosage form, or adds a device or special release system to improve how the medicine works. It’s not just a copy-it’s an upgrade.
Are generic combinations as safe as brand-name drugs?
Yes-if they’re approved. The FDA requires complex combinations to prove they’re equivalent in safety and effectiveness. But because these products are more complex, the standards for proving equivalence are still evolving. Some experts warn that current testing methods may not catch subtle differences in how the drug is delivered.
Why are generic combinations more expensive to develop?
They require advanced manufacturing, more clinical data, and longer approval times. A simple generic might cost $1-5 million and take 2-3 years. A complex combination can cost $15-50 million and take 4-7 years. That’s because you’re not just copying a drug-you’re engineering a new delivery system.
Which countries lead in manufacturing generic combinations?
India produces 35% of the world’s complex generics, thanks to low costs and strong technical skills. The U.S. leads in innovation and approvals, with 37 complex combinations approved by early 2025. The EU lags behind with only 12. The U.S. is now pushing to bring more manufacturing home with new fast-track programs.
Will generic combinations replace brand-name drugs entirely?
Not entirely, but they’ll take over large portions of the market. When patents expire, brand-name drugs face immediate price drops. Generic combinations offer a way to maintain value by improving the product. They won’t replace every brand, but they’ll dominate the high-volume, chronic disease areas where adherence and delivery matter most.

Comments
This is the future right here. No more pill organizers falling off the counter. One pill that does three things? Yes please. I’ve seen grandparents forget half their meds - this could literally save lives. 🙌
It’s fascinating how we’ve gone from ‘copy the molecule’ to ‘re-engineer the entire experience.’ The real innovation isn’t the chemistry - it’s the psychology baked into the delivery. A pill that remembers for you? That’s not pharmaceuticals anymore. That’s behavioral tech wrapped in cellulose. And honestly? Kinda beautiful.
Yeah sure, $50M development costs. But let’s be real - most of these ‘complex’ combos are just rebranding old crap with a fancy coating. FDA’s letting them skate by with weak bioequivalence data. It’s corporate greed dressed up as progress.
Okay but imagine this - a diabetic gets a pen that doesn’t just inject insulin, but also texts their doctor if their glucose spikes within 20 minutes of dosing. The device isn’t just a tool - it’s a co-pilot. And now the FDA’s got this pilot program pushing U.S. manufacturing? That’s not protectionism. That’s a reclamation of dignity in medicine. We used to make the world’s best tech. Why stop now? We’re not just making pills - we’re making peace of mind. And honestly? That’s worth every penny.
You people are naive. This isn’t healthcare innovation - it’s a money grab disguised as progress. Companies know patients won’t notice the difference between a 2% variance in release rate. So they charge 3x and call it ‘premium.’ Meanwhile, the real problem - drug pricing - stays untouched. They’re not curing disease. They’re monetizing compliance.
India making 35% of these? YES! 🇮🇳 Our engineers are quiet geniuses - no hype, just precision. And now the U.S. wants to bring it home? Cool. But don’t forget who built the foundation. Let’s collaborate, not compete. 💪❤️
USA thinks it’s smart because it approves 37 combos? Ha. India makes them cheaper, faster, better. U.S. just wants to protect its pharma cartel. This ‘fast-track’? Just a tax break for big pharma. Don’t believe the propaganda. We’ve been doing this for decades while you slept.
Wait so if a combo pill has a sensor in it… does that mean it’s like… a smart pill? Like from that movie? lol i think i read somethin bout this but i got distracted by cat videos. also i think the FDA is spelled with a C not a K? 🤔