Bone Health Medication Comparison Tool
Select Medication to Compare
Filter by Indication
Didronel (Etidronate) is a bisphosphonate used to treat Paget's disease, prevent bone loss, and manage hypercalcaemia. If you’re weighing it against newer options, you’ll want to know how it stacks up on mechanism, dosing, safety, and cost.
What Is Didronel (Etidronate)?
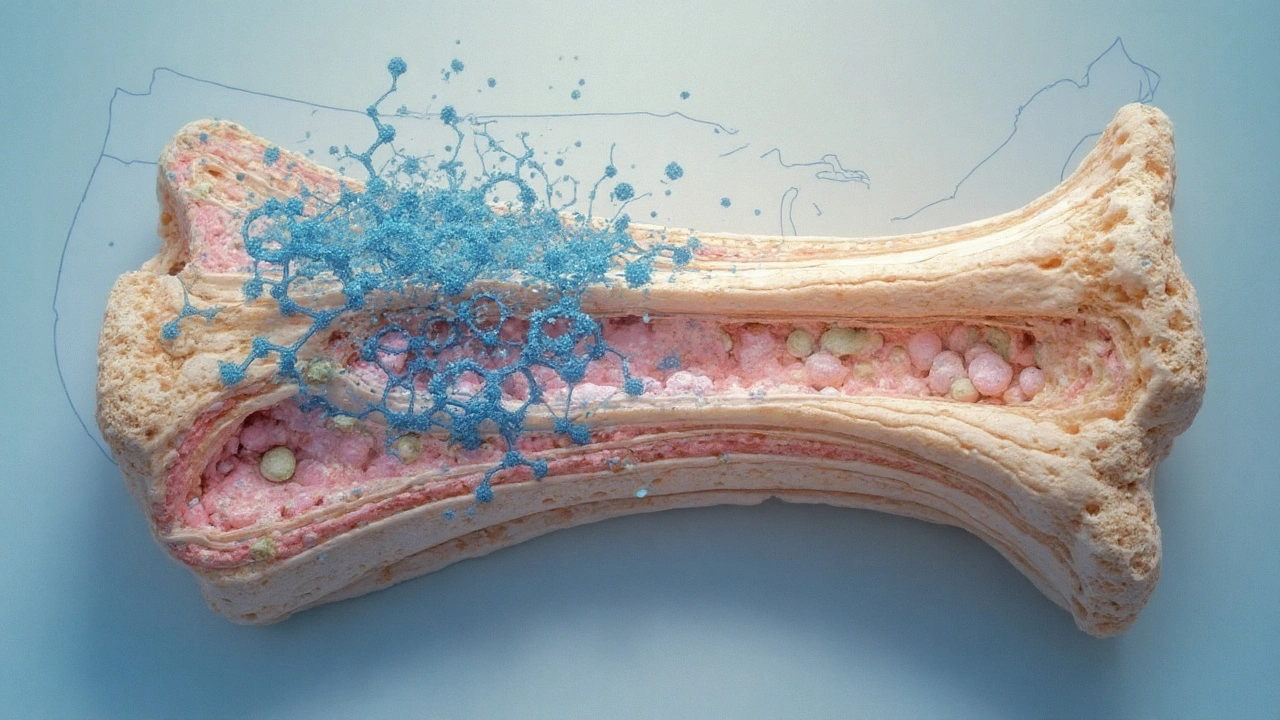
Didronel (Etidronate) is a first‑generation oral bisphosphonate that binds to hydroxy‑apatite crystals in bone, inhibiting osteoclast‑mediated resorption. It is typically prescribed at 400mg twice daily for 30 days followed by a 30‑day drug‑free interval when used for Paget's disease, or in low‑dose regimens (400mg once daily) to prevent heterotopic ossification after surgery.
Key Attributes of Didronel
- Mechanism: Inhibits the mevalonate pathway, reducing osteoclast activity.
- Administration: Oral tablets taken with a full glass of water, on an empty stomach.
- Typical dosing: 400mg twice daily (cycling) or 400mg once daily (low‑dose).
- Approved indications (US FDA, EU EMA): Paget's disease, prevention of heterotopic ossification, hypercalcaemia of malignancy.
- Notable side effects: Gastro‑intestinal irritation, oesophageal ulceration, rare osteomalacia with prolonged high‑dose use.
Why Look at Alternatives?
Didronel’s efficacy is solid, but its dosing schedule can be cumbersome and its gastrointestinal tolerance is lower than newer bisphosphonates. Moreover, many clinicians now favour agents with monthly or yearly dosing, better bone‑density outcomes, or different mechanisms for patients who can’t tolerate oral bisphosphonates.
Modern Oral Bisphosphonates
Alendronate is a second‑generation oral bisphosphonate that offers weekly dosing and stronger affinity for bone mineral, resulting in higher bone‑mineral density (BMD) gains.
Risedronate provides weekly or monthly regimens and has a favorable gastrointestinal safety profile compared with first‑generation agents.
Zoledronic acid is an intravenous bisphosphonate administered once yearly (or once for a single high‑dose treatment of Paget's disease). Its potency exceeds oral agents, delivering rapid reductions in bone turnover markers.
Non‑Bisphosphonate Options
Denosumab is a monoclonic antibody that blocks RANKL, preventing osteoclast formation. It is given subcutaneously every six months and is effective for osteoporosis, bone loss secondary to cancer therapy, and high‑risk Paget's disease.
Teriparatide is a recombinant parathyroid hormone analog that stimulates new bone formation, used for severe osteoporosis and for patients who have failed bisphosphonate therapy.
Calcitonin is a peptide hormone that directly inhibits osteoclast activity. It is available as nasal spray or injection and is often reserved for acute pain relief in Paget's disease.
Strontium ranelate works by simultaneously increasing bone formation and decreasing resorption. Though withdrawn from many markets due to cardiovascular concerns, it remains an option in some regions for patients intolerant to bisphosphonates.
Side‑Effect Profiles at a Glance
| Medication | Mechanism | Route & Frequency | Key Indications | Common Side Effects |
|---|---|---|---|---|
| Didronel (Etidronate) | Bisphosphonate - mevalonate inhibition | Oral, 400mg BID (30‑day on/off) | Paget's disease, heterotopic ossification, hypercalcaemia | GI irritation, oesophageal ulcer, rare osteomalacia |
| Alendronate | Bisphosphonate - osteoclast apoptosis | Oral, 70mg weekly | Post‑menopausal osteoporosis, glucocorticoid‑induced bone loss | Stomach upset, esophagitis, atypical femur fracture (rare) |
| Risedronate | Bisphosphonate - osteoclast inhibition | Oral, 35mg weekly or 150mg monthly | Osteoporosis, Paget's disease (high‑dose) | GI discomfort, esophagitis, hypocalcaemia |
| Zoledronic acid | IV bisphosphonate - potent osteoclast suppression | IV infusion, once yearly (or single 5mg dose for Paget's) | Osteoporosis, Paget's disease, hypercalcaemia | Acute phase reaction, renal impairment, atrial fibrillation (rare) |
| Denosumab | RANKL antibody - blocks osteoclast formation | SC injection, every 6 months | Osteoporosis, bone loss from cancer therapy | Skin reactions, hypocalcaemia, rare ONJ |
| Teriparatide | PTH analog - stimulates bone formation | SC injection daily | Severe osteoporosis, glucocorticoid‑induced bone loss | Nausea, hypercalcaemia, cost |
| Calcitonin | Hormone - directly inhibits osteoclasts | Nasal spray or injection, daily | Pain relief in Paget's disease, osteoporosis (adjunct) | Nasal irritation, allergic reactions, limited efficacy |
| Strontium ranelate | Dual action - increases formation, reduces resorption | Oral, 2g daily | Osteoporosis (where approved) | Cardiovascular risk, venous thromboembolism |
How to Choose the Right Medication
Think of the decision as a checklist rather than a guess:
- Indication specificity. Paget's disease responds well to cyclic high‑dose Didronel, while osteoporosis benefits more from weekly alendronate or six‑monthly denosumab.
- Adherence potential. If a patient struggles with daily pills, a yearly zoledronic infusion may be a game‑changer.
- Renal function. Oral bisphosphonates are safer for mild kidney disease; IV zoledronic acid requires eGFR>30mL/min.
- Gastro‑intestinal tolerance. Patients with reflux disease often prefer denosumab or subcutaneous teriparatide.
- Cost and insurance coverage. Generic alendronate and risedronate are cheap, whereas biologics like denosumab carry higher out‑of‑pocket costs.
- Future pregnancy plans. Bisphosphonates have long skeletal half‑lives; teriparatide is usually avoided in women planning pregnancy.
Practical Tips for Patients on Didronel
- Take the tablet with a full glass of water, stand upright for at least 30minutes.
- Avoid calcium, antacids, or food within 30minutes of dosing to maximize absorption.
- Schedule the 30‑day on/off cycle in your calendar; missing a cycle reduces efficacy.
- Monitor serum calcium and phosphate levels every 3‑6months, especially if using high‑dose cycles.
- If you develop persistent stomach pain or reflux, discuss switching to a weekly oral bisphosphonate or an injectable alternative.
Emerging Developments and Future Directions
Research is tweaking the bisphosphonate backbone to create agents with fewer gastrointestinal complaints while retaining bone‑targeting potency. Meanwhile, combination regimens (e.g., a short course of Didronel followed by denosumab) are under investigation for refractory Paget's disease. Keep an eye on clinical trial registries for updates-new evidence may shift the balance in favour of hybrid strategies.
Bottom Line
Didronel remains a solid choice for specific scenarios like Paget's disease and short‑term hypercalcaemia control, but its dosing schedule and GI profile often make newer oral bisphosphonates, IV agents, or biologics a better fit for chronic osteoporosis management. By matching the drug’s mechanism, route, and side‑effect profile to a patient’s lifestyle and comorbidities, clinicians can optimise bone health while minimising hassle.
Frequently Asked Questions
What is the main advantage of Didronel over newer bisphosphonates?
Didronel’s quick‑acting effect on bone turnover makes it useful for rapidly lowering calcium levels in malignancy‑related hypercalcaemia and for short‑term control of Paget's disease, where high‑dose cyclic therapy is required.
Can I switch from Didronel to alendronate without a wash‑out period?
Because both are bisphosphonates, a short wash‑out (usually 7‑10days) is advisable to reduce the risk of overlapping gastrointestinal irritation. Your doctor will check kidney function before making the change.
Is Didronel safe for people with reduced kidney function?
Oral Didronel is generally safe down to an eGFR of 30mL/min, but higher doses can accumulate in bone and may exacerbate renal impairment. Always have serum creatinine checked before starting long‑term therapy.
How does denosumab compare to Didronel for osteoporosis?
Denosumab provides more consistent BMD gains, works in patients who cannot tolerate oral bisphosphonates, and is given only twice a year. However, it requires regular injections and has a rebound bone loss risk if discontinued abruptly, unlike the long skeletal residence of Didronel.
What are the warning signs of osteomalacia with long‑term Didronel?
Persistent bone pain, muscle weakness, and low serum calcium/phosphate levels may signal over‑suppression of bone turnover. If they appear, stop the drug and start vitamin D and calcium supplementation under medical supervision.


Comments
so didronel is just the gateway drug of bone meds lol
next thing you know you're on denosumab and wondering why your bones are still breaking
the pharmaceutical industry doesn't want you to know that bones heal themselves if you just stop eating processed food and start walking barefoot on grass 🌱🪴
This whole article is a CIA psyop to get old people hooked on pills so they don't revolt against the system.
Fascinating breakdown! As a clinical pharmacist in Lagos, I've seen patients on Didronel struggle with adherence due to the strict dosing protocol - especially in rural areas where refrigeration and clean water access are inconsistent. The shift toward denosumab or zoledronic acid in our setting isn't just about efficacy - it's about practicality. We're seeing 78% better compliance with quarterly IV infusions versus cycling 400mg BID. Also, let's not ignore cost: generic alendronate at $0.12/day versus denosumab at $1200/month? The math speaks louder than the marketing.
why is everyone so obsessed with bones anyway like i just want to eat pizza and not think about my skeleton
I love how this article casually mentions strontium ranelate like it's still a viable option. It was pulled from the EU and Canada because it turned people's hearts into ticking time bombs. And now we're supposed to trust these 'hybrid strategies' with people's lives? This isn't medicine - it's a casino where the house always wins, and the patients pay with their kidneys.
The 30-day on/off cycle for Didronel is brutal but necessary - missed doses = reduced efficacy
Most patients don't realize you can't just take it with coffee or calcium
Also - if you're on it for Paget's, monitor ALP levels every 3 months, not just calcium
You know what’s really ironic? We’ve spent decades optimizing bone drugs to fight osteoporosis - while the real problem is that we’ve stopped *living* like animals. We sit. We don’t jump. We don’t carry heavy things. We don’t run from predators. We don’t get sunlight. We don’t eat real food. So we take pills to fix what we broke by living like zombies. Didronel? It’s just a Band-Aid on a corpse. The real treatment is a hike in the woods, a squat, and a sunset. But no - let’s just inject more money into Big Pharma’s vaults.
The clinical utility of Didronel remains statistically significant in the context of Paget’s disease management, as per the 2021 Cochrane meta-analysis. However, the risk-benefit ratio, particularly concerning osteomalacia and gastrointestinal toxicity, necessitates a paradigmatic shift toward agents with more favorable pharmacokinetic profiles. The current literature overwhelmingly supports the adoption of RANKL inhibitors in long-term osteoporotic regimens, particularly in geriatric populations with comorbid gastrointestinal pathology.
Oh wow, so we're supposed to be *impressed* that a 1970s drug still exists because it 'works'? Meanwhile, my aunt got osteonecrosis from denosumab and now she's on morphine. But hey - at least it's 'biologic' and sounds fancy on a billboard. 🙄
ok so i just found out my grandma was on didronel and she said it made her feel like her bones were turning to dust?? like?? why is this even a thing?? i thought bones were supposed to be strong?? 🤯
If you're on Didronel, don't give up - it's tough but it works
Stay upright after taking it
Set phone alarms for the 30-day cycle
You got this 💪
In Nigeria, access to bone health meds is a real challenge. Many patients rely on traditional healers or self-medicate with calcium supplements from roadside vendors. Didronel is often unavailable or too expensive. But when it is available, and when patients are properly counseled on the dosing schedule - especially the mandatory drug-free interval - outcomes are surprisingly good. We've even started using community health workers to remind patients via WhatsApp. Technology meets tradition. And yes, the 400mg BID cycle is a pain, but it's better than a fractured hip at 65. Keep pushing for awareness - bone health is silent until it screams.
I'm so glad this exists 🙌
My mom had Paget's and didronel saved her from needing surgery
But honestly? The hardest part was remembering to stand still for 30 mins after each pill 😅
Now she's on denosumab and she says it's way easier - no more calendar alarms 📅❤️